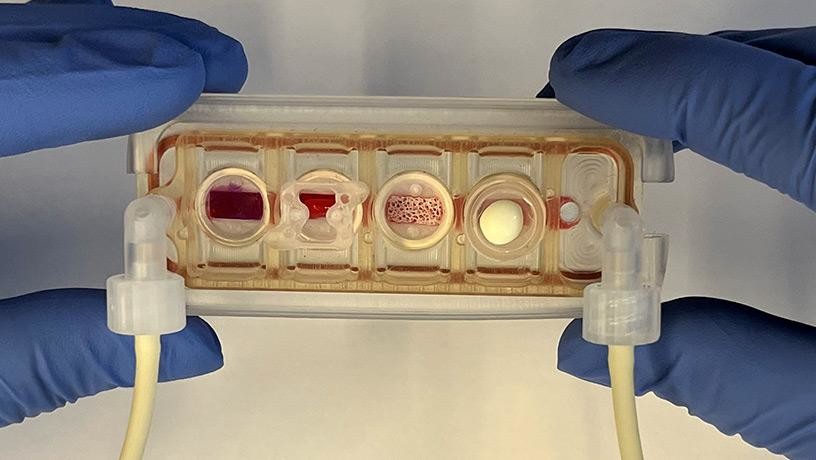
A team of Columbia biomedical engineers has developed a remarkable new “organs-on-a-chip” technology: a simulation of our most important human tissues, connected by a bloodstream, which will enable doctors to test whether a drug will be safe and effective for a given person. The engineers say the device could lead to more personalized treatments for cancer and other diseases.
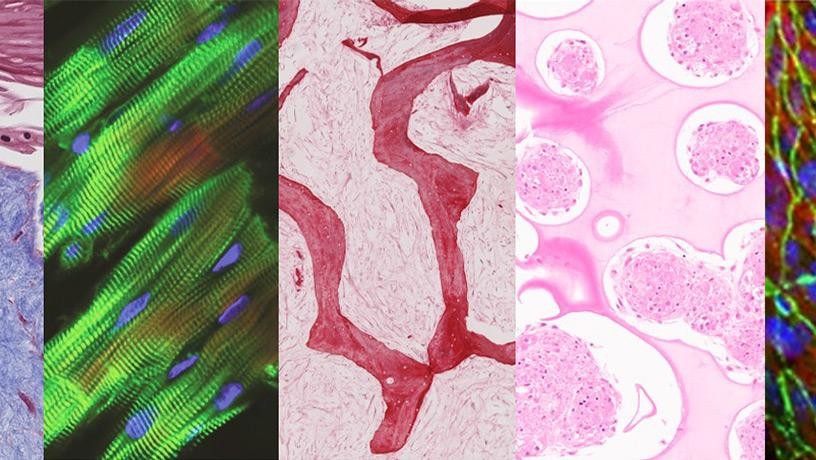
In a paper published recently in Nature Biomedical Engineering, the researchers describe how they have managed to grow human heart, skin, bone, and liver tissues using a patient’s own stem cells and keep these organ fragments alive for weeks in a plastic device the size of a credit card. Here the tissues communicate with each other through a shared blood supply replete with circulating immune cells, cytokines, and other bioactive molecules.
The system, which was in development for more than a decade, provides scientists and physicians with their first up-close look at how different types of human tissues interact in real time.
“This is especially important for studying diseases like cancer or viral infections that can spread throughout the body and afflict multiple organs,” says Gordana Vunjak-Novakovic, a University Professor and a specialist in biomedical engineering, medical sciences, and dental medicine, who led the research team.
Vunjak-Novakovic and her colleagues, together with a group of Columbia biologists led by Andrea Califano, are currently using their new system to study the basic biology of cancer, investigating how malignant cells that arise in one organ can hitch a ride on the bloodstream and invade others. But the technology has more immediate clinical applications, since it can also be used to predict how individual patients are likely to respond to medications before taking them.
“With our technology, researchers can determine which medications are safest for a patient, based on how their lab-grown tissues tolerate various drug options,” says Vunjak-Novakovic.