Walter Bockting, a clinical psychologist and the founding director of the Gender and Sexuality Program at Columbia University Irving Medical Center (CUIMC), explains why more young people are identifying as transgender and discusses issues surrounding care.
Tell us about the Gender and Sexuality Program. What is its mission? Who does it serve?
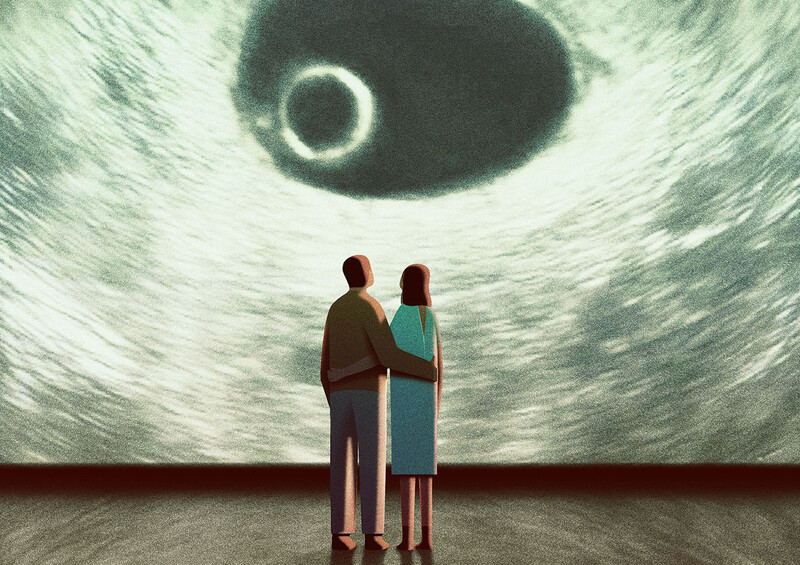
We launched our program in 2018 to serve people identifying as transgender or nonbinary. It now offers comprehensive mental-health services to those who are questioning their gender or sexuality or struggling to navigate life with an identity that does not conform to traditional expectations. The majority of our patients are adolescents and teenagers, some of whom are considering medical treatments to align their bodies with their gender identity. We also see adults who are considering making such changes. And sometimes parents will come in with young children who appear to identify with another gender. They want to understand what their children are going through and how best to support them.
What exactly do the terms “transgender” and “nonbinary” mean?
Transgender is an umbrella term used to describe anyone with a gender identity that differs significantly from the sex they were assigned on their birth certificate, based on their outward anatomy. This can include people whose gender is the opposite of the sex they were assigned at birth — that is, a person assigned male at birth who identifies as a girl or woman or a person assigned female at birth who identifies as a boy or man. Transgender people may undergo medical interventions to align their appearance with their gender identity, or they may choose not to do so. Nonbinary individuals, who identify as neither boy nor girl, man nor woman, are generally considered part of the transgender community too. Their identities may combine aspects of masculinity or femininity or transcend these binary categories. Research conducted by my group and others has shown that gender identity and expression exist on a spectrum. For many people they are composed of different characteristics not easily reducible to being either male or female, masculine or feminine.
Is the transgender population growing?
There’s been a significant increase in people who openly identify as transgender or nonbinary over the past decade, especially among young people. Surveys indicate that 2 to 3 percent of adolescents and teenagers and about 5 percent of young adults in the United States now identify as transgender, with half or more of these individuals considering themselves nonbinary. Among older adults, that number is less than 1 percent, which is in line with historical trends dating back to the mid-twentieth century, when the concept of gender identity as distinct from biological sex first emerged.
What explains the rise?
Of course, there are cultural forces at work. As more and more people have embraced diverse gender identities, less stigma is associated with being trans. Which isn’t to say that it’s particularly easy to come out as transgender, because gender-nonconforming people are still among the most stigmatized in society. But transgender people feel freer to be themselves now, compared to previous decades. This is especially true for young people who’ve grown up seeing transgender individuals depicted positively in the media and meeting other transgender folks in school, on the job, or through friends and family. I think that older adults who grew up when it was less socially acceptable to be transgender are more likely to have suppressed or concealed any gender-identity issues they had, which is why you see a generational divide in these statistics.
How many Americans now undergo gender-affirming surgeries?
It’s difficult to say for sure, because the US has no centralized system for collecting data on such procedures, but it’s probably on the order of ten thousand people a year, the vast majority of whom are adults. Only a few hundred adolescents undergo gender-affirming surgeries annually, although thousands of young people do receive puberty suppressants or hormones to feminize or masculinize their bodies.
Before they perform gender-affirming surgery, physicians typically require a referral from a mental-health professional who can attest that a patient has thought the decision through, and in the past obtaining such a referral was more challenging than it is today. For example, until the mid-1990s, people who sought genital surgery were often turned down if they exhibited symptoms of severe anxiety or depression, which were seen as signs of mental instability. Now we know that feeling an incongruence between one’s gender identity and sex assigned at birth can contribute to mood disorders and that it is often appropriate to provide a person gender-affirming care at the same time that you’re treating them for other mental-health conditions.
People who opt for gender-affirming surgeries typically carry a diagnosis of gender dysphoria, a condition characterized by a discomfort with one’s sex assigned at birth that is so intense that it becomes debilitating, making daily life difficult if not impossible. Many, but not all, teenagers and young adults who now identify as transgender experience gender dysphoria. And having gender dysphoria does not necessarily lead a person to seek puberty suppression, hormone therapy, surgery, or any other gender-affirming medical interventions. Gender dysphoria plays out differently for each person.
Do your patients at the Gender and Sexuality Program tend to have dysphoria?
Most of them do, yes. We see people who are in a lot of emotional pain. In addition to experiencing incongruence between their gender identity and physical sex characteristics, which is incredibly frustrating, many are also socially isolated. Before coming to us, some have never spoken to anybody at length about what they’re going through. They might also have experienced bullying, harassment, violence, and discrimination. And it’s not uncommon for them to have internalized other people’s negative attitudes about transgender people and to feel ashamed of who they are. The cumulative stress can contribute to a wide range of mental-health issues, including substance abuse, suicidal thoughts, self-harm, anxiety, and mood disorders. When we help them come up with a plan to alleviate their gender dysphoria, we often need to address these issues, too.
What does treatment typically look like?
It starts with talk therapy to facilitate self-acceptance and identity exploration. We ask patients to describe how they’d ideally like to express their gender and what, if anything, is holding them back. If they haven’t lived openly as a transgender person yet, we might suggest that they first learn about the possibilities online and then try expressing their gender identity in a safe, private setting, like in the company of supportive friends or family members. After exploring their identity and expression in this way, some people may decide that they don’t need to change their gender identity in a formal sense. They might conclude that they’re simply uncomfortable with traditional gender norms and can be happy continuing to identify as a man or woman if they bend the rules to their liking a bit. But more often than not, among the patients we see, such experiences are affirming, encouraging people to move forward and continue transitioning. Then we might help them develop a plan for coming out at school or work, which can include preparing to address changes in pronoun use, how they dress, and bathroom access. We’ll work with their families to ensure that individuals get the emotional and social support they need. And if a patient is determined to change their body, we’ll help them think through the available options. We’ll also support them after they’ve made any physical changes, because the challenges of being transgender don’t end at that point.
You’ve been counseling transgender people and studying their lives for more than three decades. In particular, you’ve researched how their identities evolve over time. What have you learned?
One insight is that most transgender people, as they get older, become less interested in trying to pass as cisgender men and women and more comfortable identifying primarily as trans men, trans women, or nonbinary individuals. It can take them years to get to this point, because many transgender people, especially when they’re young, have internalized our society’s binary conception of gender and feel compelled to adopt the stereotypical gender expressions of men or women. They may initially think, “Well, I know I’m not a girl, so I must be a boy. Now I need to look and behave exactly like one!” This isn’t surprising. It’s human nature to seek a sense of belonging by carving out rather neatly defined identities for ourselves. And realizing that your gender identity is different or ambiguous can be nerve-racking. When my colleagues and I counsel transgender people, we encourage them to unearth and face some of this anxiety. We’ve found that by accepting the complexity and uniqueness of their gender identities, and by embracing the fact that, as transgender people, their experiences will always be unique and a bit different from cisgender people’s, they’re able to feel better about themselves and ultimately find more meaning in their lives.
Shortly before coming to Columbia in 2012, you served as president of the World Professional Association for Transgender Health (WPATH). In that role, you oversaw the creation of treatment guidelines that have made it easier for nonbinary people in many countries to access appropriate gender-affirming medical care.
Yes, these guidelines, which are now followed by most medical professionals and endorsed by their associations, stipulate that people who identify as nonbinary should have access to the same high-quality care as other transgender people. This is important because, as recently as the early 2000s, people who needed to change their bodies but didn’t necessarily want to look like cisgender men or women were often turned away. Maybe they just wanted to alter their chest, tone of voice, or hair-growth patterns while forgoing other procedures. If a physician asked if they identified as a man or woman and they responded, “Neither,” they might have been told, “Well, come back when you figure it out.” Now they’re treated equally and can access gender-affirming medical interventions appropriate to their identities and needs.
You’re also credited with improving access to care for transgender people who identify as gay, lesbian, or bisexual.
Yes, when I entered this field, another common requirement for getting gender-affirming surgery was to identify as heterosexual after transitioning. Can you believe that? In other words, you couldn’t be sexually attracted to members of your own gender identity but rather only to members of the sex you were originally assigned at birth. This was rooted in a twentieth-century theory called the “inversion hypothesis,” which held that the desire to transition one’s gender was the manifestation of intense same-sex attraction — basically, an extreme form of homosexuality. So, for example, a person who was assigned male at birth and sexually attracted to other men — and who had an unusually “de-masculinized and feminized” mind — might eventually want to become a woman. Transgender people who were brave enough to disclose their same-gender attractions faced significant barriers to accessing gender-affirming medical care. And transgender men who were attracted to men weren’t even thought to exist. But in the late 1980s and early 1990s, I published a series of papers documenting that transgender men who are attracted to men do exist and are quite happy and well-adjusted. This research, together with other scholars’ observations that transgender women often identify as lesbian, helped usher in a paradigm shift, where gender identity and sexual orientation were finally understood as separate components of one’s overall identity.
Today there is fierce debate about whether it has become too easy for adolescents to access gender-affirming medical care. In the past couple of years, more than twenty states have passed laws banning anyone under the age of eighteen from receiving puberty suppressants, hormone therapies, and surgeries. What do you make of this?
I’m shocked at how thoroughly the public discussion on this issue has become politicized and inundated by misinformation. Opponents of transgender rights, who’ve now organized themselves into a powerful movement, would have Americans believe that their kids are being brainwashed into thinking they’re transgender and greenlighted for medical procedures that they don’t need and will later regret. Of course, this isn’t true. Even among youth with gender dysphoria, only those with the most pronounced symptoms access medical interventions, usually after extensive counseling and therapy. What’s really happening is that young people in nearly half the United States are being denied access to health care that they desperately need, care that nearly every major medical organization in the country has deemed safe and essential. It’s a disgrace. Honestly, it makes me so upset that it’s difficult for me to talk about it.
“I’m shocked at how thoroughly the public discussion on this issue has become politicized and inundated by misinformation.”
When you meet a young person with gender dysphoria and hear them describe what they’re going through, you don’t forget it. It’s heartbreaking. I’m talking about kids who are overwhelmed by despair related to their sex characteristics. Who take showers in the dark to avoid seeing their bodies. Who can’t focus in school because they’re so upset about going through puberty. To these kids and their families, having access to gender-affirming care can feel like a matter of life or death.
Puberty blockers are now given to transgender kids as young as ten or eleven, which critics point out is a pretty tender age to be making medical decisions whose effects could last a lifetime.
Helping kids to change their bodies raises serious questions and concerns, there’s no doubt about it. I think that everyone working in the field of transgender health right now is asking themselves: Will any of these kids come to regret this decision? Will the puberty blockers cause any unintended effects later in life? Exactly how much therapy should these kids be getting before they transition? We don’t have conclusive answers to these questions
yet. The best data available comes from a clinic in Amsterdam where gender-affirming medical care was first provided to adolescents in the 1990s. I grew up and trained in the Netherlands, and I’ve conducted research with some of the people who developed that program, which has shaped my thinking. In any case, the results from patients of that clinic are so far positive, which is why health-care providers throughout Europe and the US have since started offering puberty suppression and hormone therapies to adolescents. Hundreds of Dutch people who received gender-affirming care as youngsters decades ago are still being followed by researchers. Very few say they regret transitioning or show signs of serious unintended effects. And as a group, they have lower rates of anxiety and depression than other transgender people who attain access to gender-affirming care later in life or not at all.
What are you studying now?
For the past eight years, I’ve been leading a longitudinal study following the lives of more than three hundred transgender people, who now range in age from about twenty to ninety, in New York City, San Francisco, and Atlanta. My colleagues and I are hoping to follow these participants for years to come. We want to learn what aspects of their lives are most challenging, what brings them happiness and contentment, and how they develop resilience in the face of stigma, discrimination, and the associated stress. Among our discoveries so far is that transgender people who maintain close friendships with other transgender people are happier and healthier overall, as are those who are in regular contact with their parents, siblings, or other close family members and friends.
The importance of family, I think, is particularly interesting. Other studies have shown that transgender people are often rejected by their families or subjected to such awful abuse at home that they have to cut ties. Some of our participants have experienced this too. But many others told us things like, “You know, my folks weren’t very nice to me at first and actually said some terrible things. But I was patient and left the door open, and eventually they came around and accepted me. And I’m glad I gave them a chance, for my own sake and theirs.”
That’s inspiring. Do you share those types of stories with your patients?
I do. I’m always telling my patients about the dignity, strength, and courage of other transgender people. I’ll recommend movies, TV shows, and books, and I’ll tell them anecdotes about some of the amazing patients and research participants I’ve known over the years. When they’re ready, I’ll help them connect meaningfully with other transgender people in group therapy and support meetings. And I’ll tell them, “I know that being transgender isn’t easy — but it’s also exciting, beautiful, and, yes, fabulous. And you are now among these fabulous people who, just by being themselves and holding their heads up high, are changing the world.”
This article appears in the Winter 2023-23 print edition of Columbia Magazine with the title "Beyond the Binary."