For dermatologist Robyn Gmyrek, it was the cruelest fate: After she had spent years performing cosmetic procedures on people with warts, acne, scars, and crow’s feet, in 2002 her own face erupted with lesions that itched and burned and caused her to claw at her skin until it was raw. “The suffering was beyond,” says Gmyrek, an assistant clinical professor at Columbia University Medical Center (CUMC). “It felt like my skin was on fire.”
What to tell her patients? Would they trust a dermatologist incapable of caring for her own complexion? “I was honest with them,” she says. “I told them I didn’t know what it was. Most patients were understanding. But it was difficult to go to work.”
Other doctors were puzzled by Gmyrek’s condition, too. They wondered if she might have an allergic reaction to chemicals commonly found in the air, or even lupus. They gave her steroids, antibiotics, and herbal remedies. Nothing worked. In fact, Gmyrek’s condition worsened over the next year, spreading to 70 percent of her body and forming open sores.
Eventually, Gmyrek began to suspect that she had a rash that stems from celiac disease, which is a severe allergic reaction to a protein called gluten that’s found in wheat, barley, and rye. Her dermatological symptoms matched. And yet something didn’t fit: Gmyrek recalled learning in medical school that all patients with celiac disease have chronic diarrhea, abdominal pain, and weight loss. That would figure, since celiac disease occurs when the small intestine, upon mistaking gluten for a toxin, attacks its own lining to diminish its absorptive power and thus seal off the rest of the body from the threat. Gmyrek didn’t think she had any digestive problems.
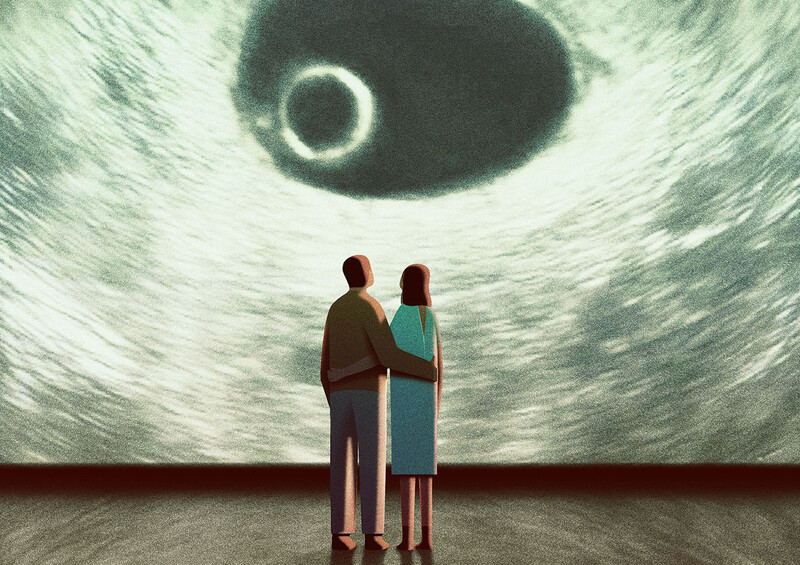
Nevertheless, she made an appointment at Columbia’s Celiac Disease Center, which is directed by Peter H. R. Green, one of the country’s top experts on the disorder. Green recognized her skin condition as dermatitis herpetiformis, whose only known cause is celiac disease. It occurs when skin cells attack themselves in a sort of autoimmune aftershock to the intestine’s self-destruction. Green performed a biopsy on Gmyrek’s small intestine a few days later to confirm she had celiac. “When I got out of anesthesia, Peter was there, and I could tell that he was excited,” says Gmyrek. “He told me I had one of the worst cases he’d ever seen.”
Why no diarrhea or abdominal pain? “That’s a misconception many doctors have,” says Green, an Australian-born gastroenterologist who speaks brusquely and with a rough-hewn accent. “Medical textbooks in the United States teach it wrong. That’s a big problem.” Only one in six people with celiac disease, he says, experience unusual gastrointestinal discomfort.
Gmyrek’s treatment was straightforward, if arduous to abide, as is always the case for celiac: She needed to follow a gluten-free diet for the rest of her life. So she cut out wheat in favor of alternatives like flax, oats, quinoa, teff, and buckwheat. Within a month, her rash started to fade, and a year later, it had disappeared for good. “I feel very lucky,” she says.
Gmyrek is one of the few people with celiac disease in the United States today who are fortunate enough to be diagnosed. An estimated 3 million Americans — about 1 in every 100 — has celiac disease, yet 97 percent of them don’t know they have it, according to Green, coauthor of the 2006 book Celiac Disease: A Hidden Epidemic, which will be published in an updated edition by HarperCollins in January. Moreover, the prevalence of the disease is increasing: The percentage of Americans with the disorder has increased fourfold in the past 50 years, for reasons that are unclear to scientists.
Fortunately, few people with celiac disease experience symptoms that are as painful as Gmyrek’s. But that doesn’t mean their health situations are less critical. Most people with celiac disease will at some point be treated for a serious condition that stems from the breakdown of their small intestine, usually by a physician who is unaware of the underlying inflammation, Green explained recently in his office at CUMC. He ticked off a partial list of health problems that can result from celiac: osteoporosis, anemia, chronic fatigue, weight loss, diabetes, attention deficit disorder, arthritis, migraines, seizures, numbness, infertility, depression, and intestinal cancer.
Celiac disease is a master of disguise because it may strike any section of the small intestine, with each section being responsible for the absorption of different vitamins and minerals and associated with different biochemical changes in the body. Even the most diligent doctors have difficulty spotting it. “Yet in Finland, they catch 70 percent of all cases, and in Italy, Ireland, and Australia, they spot an estimated 30 to 40 percent of cases,” says Green. In Europe, dermatologists are trained to consider celiac as a potential source for skin conditions, he says, just as hematologists know that celiac is a possible explanation for anemia and neurologists know it can cause numbness.
Why are U.S. physicians spotting only 3 percent of cases? Part of the problem is that celiac disease, because it’s treatable without drugs, hasn’t attracted much attention from medical researchers in the United States, says Green. Drug companies pay for 80 percent of all medical research in this country, he points out.
“If drug companies don’t think there’s money to be made treating celiac disease,” Green says, “doctors aren’t going to see many research papers about it, they’re not going to hear lectures about it at the big medical-education conferences sponsored by drug companies, and they’re certainly not going to have attractive ex-cheerleaders showing up at their office doors with samples of gluten-free food, asking them how many people they diagnosed with celiac this week.”
The secret life of wheat
The Greek physician Aretaeus of Cappadocia is credited with identifying celiac disease, having written in the first century AD of a “coeliac affection” that made the stomach “irretentive of food.” He named it after the Greek word for abdomen, “koelia.”
The disorder had probably appeared 8,000 to 12,000 years earlier. That’s when humans, hunter-gatherers until then who survived on fruits, nuts, and the sporadic feast of meat, began cultivating crops, Green writes in A Hidden Epidemic. In this era, people in what is now Syria crossbred several types of wild grass to produce a large and nutritious grain, wheat. Wheat proved ideal for making bread because it gets sticky when mixed with water, a quality derived from gluten, which is a protein made of an unusually long peptide chain of 33 amino acids. Humans don’t have digestive enzymes to break down gluten’s complex molecular structure, but the protein is expelled harmlessly from most people; it’s flagged as an intruder only in those with an overly cautious immune system.
Scientists in the late 19th century first noticed a link between carbohydrates and celiac disease. (Rice and bananas were recognized as safe and so patients were encouraged to eat lots of them.) In the 1940s, the dietary basis of the condition became clearer when the Dutch physician Willem-Karel Dicke observed that, during bread shortages caused by World War II, many sick children in his country felt better. Dicke and other scientists soon pinpointed gluten as the culprit behind celiac disease.
By the 1970s, doctors had acquired the tools they needed to diagnose celiac, Green writes. Blood tests could spot gluten-specific antibodies and a painless intestinal biopsy procedure would reveal the condition’s signature anatomical damage: On the inner wall of the small intestine, villi, microscopic protrusions that stand plump and erect to absorb nutrients when healthy, instead would be flat and shriveled.
These diagnostic advances changed the way doctors viewed celiac disease, which is also called sprue. Prior to the 1970s, celiac disease was considered a rare childhood disorder because its gastrointestinal symptoms, such as diarrhea, tended to be most severe and recognizable in young children, when they occurred at all. But as medical technology enabled doctors to detect celiac disease in the absence of these symptoms, physicians realized that the disease was a lot more common than they had previously suspected.
Doctors in Europe were the best at diagnosing celiac disease back then, just as they are today. The science journalist David P. Hamilton has documented why: Countries such as Britain, Italy, Finland, and Sweden, which have nationalized health-care systems and invest large amounts of money in preventive care, trained doctors to look for the condition. As doctors made more diagnoses, patient advocacy groups sprouted up to demand government research, which further heightened doctor awareness.
Green attended medical school in the 1970s in Sydney, where the education system has ties to England’s. “In Australia,” he says, “celiac was a part of our everyday thinking.”
So when Green arrived in the United States for a research fellowship at Harvard Medical School in 1976, he was shocked to discover that U.S. physicians still regarded celiac disease as a rare disorder that mainly struck youngsters. “In the research setting,” he says, “no one ever talked about celiac disease because there were no opportunities to study it.” And among clinicians, a cycle of ignorance had taken root: Doctors rarely met anybody who’d been diagnosed with celiac, so they continued to regard it as a medical oddity not worth learning about.
Spotting bad labels
Green has been practicing gastroenterology at Columbia University Medical Center since 1981, and in that time he has diagnosed and treated about 2000 people with celiac disease. He launched the Celiac Disease Center at Columbia, a full treatment, and research operation that employs three full-time doctors and a nutritionist, in 2002.
“I didn’t set out to be an expert at this,” Green says. “I was just doing my job as a gastroenterologist, ordering plenty of blood tests and endoscopies to look for celiac. Along the way I developed a reputation for diagnosing it and I started getting lots of patients by word of mouth.”
First-time patients often arrive at Green’s office frustrated and distrustful of doctors. “These are people who have collected doctors and wrong diagnoses,” he says. “They’ve been told that they have irritable bowel syndrome, perhaps, and so every doctor they see afterwards looks down at his chart and says, ‘OK, Mrs. Smith, how are you managing your irritable bowel syndrome lately? Not well? Oh well, yes, it’s a difficult condition. You need to be more diligent, blah, blah, blah.’”
Over the years, many of Green’s patients have made their medical records available to be studied anonymously, leading the Celiac Disease Center at Columbia to amass one of the country’s largest databases of clinical information on celiac disease. Patients have also given financially to support the center’s research mission, which has enabled Green to become a prolific study author.
In fact, to read the titles of the some 100 papers Green has authored is to survey almost all of the major questions related to the disease’s clinical presentation. Green’s work has helped demonstrate, for example, that very large numbers of celiac patients have thin bones and iron deficiency; that people with celiac have a twofold risk of developing intestinal cancer; that some of the worst health problems associated with celiac disease affect patients with no obvious gastrointestinal symptoms; that a gluten-free diet enables the small intestine to repair itself in all but the most severe cases of celiac disease; and that nonwhite people often develop celiac despite a misconception, common among doctors both in Europe and in the United States, that celiac is a Caucasian disease.
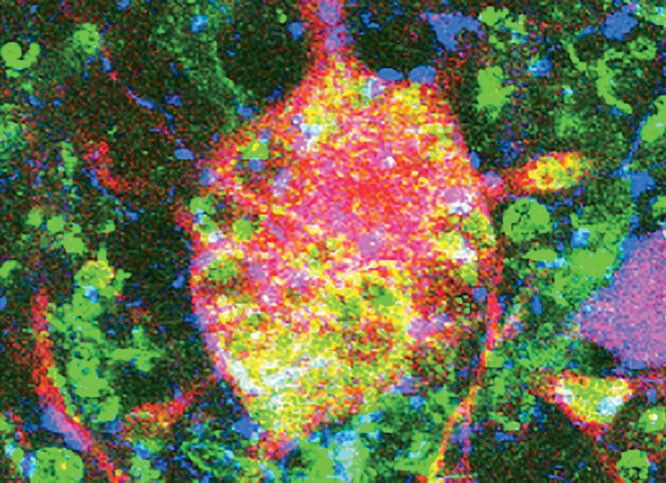
Green also has contributed to the most profound insight into celiac disease in the last half century: that much of its damage doesn’t involve poor digestion at all. Research by Green and others suggests that the small intestine’s inflammatory response can prompt other parts of the body to attack themselves, too, as happened to dermatologist Robyn Gmyrek. Green has helped demonstrate that people with celiac disease have unusually high rates of autoimmune diseases, such as type 1 diabetes, arthritis, Graves’ disease, which attacks the thyroid, and Sjögren’s syndrome, which destroys the mucous glands.
“Nearly 30 percent of the celiac patients I’ve seen have another autoimmune disorder, compared to 3 percent of the general population,” Green says. “A gluten-free diet will often lessen the severity of their other disease symptoms.”
Doctors have long observed that autoimmune diseases travel in packs; patients with one of these disorders, therefore, are usually tested for others. But American physicians have been slow to recognize that celiac disease is an autoimmune disorder, instead continuing to regard it simply as a digestive ailment, according to Green. He says this contributes to a lack of screening among people with disorders such as type 1 diabetes, who might unknowingly fuel their illness by eating wheat.
Interestingly, celiac disease is the only autoimmune disorder for which scientists have identified the primary environmental trigger. Scientists know of behavioral factors that contribute to other autoimmune disorders, such as how poor diet influences diabetes, says Govind Bhagat, a Columbia associate professor of clinical pathology who studies celiac disease. But in the case of diabetes, for example, it is suspected that a virus must also weaken the pancreas, and no one’s identified that virus yet. Celiac disease, therefore, provides a unique window into the mechanics of autoimmunity. Scientists know its trigger is gluten, and Bhagat and his colleagues now are asking: Why does the immune response seem to spread to other parts of the body? Are the attacker cells in the small intestine actually migrating? Or do biochemical changes in the small intestine signal to other organs that they should stop regulating their own immune cells?
Give them not their daily bread
Today, gluten-free food represents a $1.8 billion annual market in this country. That’s grown 25 percent in each of the past four years. Walk down the aisles of a Whole Foods and the universal symbol for gluten-free food — a wheat stalk with a slash through it — appears on hundreds of breads, pastas, pot pies, pizzas, crackers, cookies, muffins, beer, and even cosmetics.
Medical schools in the United States are updating the way they teach celiac disease. At Columbia University Medical Center, Green has trained colleagues to keep an eye out for celiac disease and he delivers an annual lecture that all students are encouraged to attend.
The typical American doctor remains uninformed, however. About 75 percent of all patients now diagnosed at the Celiac Disease Center arrive not by physician referrals, but because patients learned about Green’s practice by searching the Internet or through a patient advocacy group. That shouldn’t be surprising, though, because Americans with celiac wait an average of 11 years before they’re properly diagnosed, as Green concluded in a recent paper.
The total number of people who have celiac disease seems to be increasing dramatically. One study conducted recently at the Mayo Clinic in Rochester, Minnesota, and based on analyses of old, preserved blood samples, suggests that since 1959 the prevalence of celiac disease in this country has increased from 1 in 400, to 1 in 100. A major study in Finland in 2004 found the same rate of increase over that period. In both countries, diabetes rates also increased fourfold. A widely discussed hypothesis, offered first by the British epidemiologist David P. Strachan, is that people are becoming more prone to autoimmune disorders like diabetes and celiac disease because children are exposed to fewer germs and bacteria than in the past. This might stunt the development of the immune system, say many scientists.
“What’s really tricky is that the additional celiac cases that we’re seeing are the kind most difficult to spot,” says Green. “They’re the subtler cases, the ones where people don’t have any obvious gastrointestinal symptoms.”
Celiac disease is transforming itself into a more sneaky illness, Green believes, in part because women around the world are breastfeeding their children at higher rates than they did a few decades ago. Research suggests that a child who is breastfed is less likely to develop celiac disease — and for this reason Green definitely recommends it — yet breastfeeding also diminishes the likelihood that a youngster with celiac disease will show the types of obvious gastrointestinal symptoms that, ironically, help doctors spot the condition.
“You can understand why lots of cases are missed,” Green says. “And the only way that’s going to change is if patients take charge of their own care. If they suspect they have a problem with gluten, they need to go to their internist and say, ‘Is it possible I’ve got celiac disease? Why don’t you test me? Why don’t you refer me to somebody who treats this?’ We’ve got to talk up this disease.”