Autism is, for the most part, an inherited disorder: scientists estimate that up to 80 percent of a child’s risk of developing it is determined by DNA. But environmental and behavioral risk factors may also play a role, and since rates of autism in the US are at an all-time high, new and expecting parents are eager to learn more about the roots of this complex condition.
For the past two decades, a team of researchers including Michaeline Bresnahan ’99PH, Mady Hornig, W. Ian Lipkin, and Ezra Susser ’74CC, ’82VPS, ’93PH, all epidemiologists at Columbia’s Mailman School of Public Health, has been searching for nongenetic clues to explain why some kids develop autism and others do not. The researchers, in collaboration with the Norwegian Institute of Public Health and other Columbia scientists, have scrutinized the medical histories of more than one hundred thousand children, as well as those of their parents. Armed with unprecedented amounts of data, the researchers are investigating dozens of hypothesized risk factors for autism — everything from parental age to maternal infections to vitamin deficiencies. Columbia Magazine recently spoke to Hornig, who is herself the mother of an adult son with autism, about the team’s research.
What are the major risk factors for autism?
Well, a father’s age, which was one of the first risk factors identified a couple of decades ago, is certainly consequential. My colleague Ezra Susser published a major study on this subject in 2006. Using data collected in Israel, he showed that men who become fathers when they’re over the age of forty are six times more likely to have a child with autism than men who father kids before turning thirty. In 2016, I coauthored a larger study, which analyzed our Norwegian data together with information from Israel and three other countries, that confirmed the impact of paternal age while adding some new twists. We discovered that women at the beginning or end of their childbearing years — those in their teens or in their forties, roughly — are also more likely to have children with autism. And the biggest risk here is when older men have children with much younger women. There may be something about the big mismatch in age that can disrupt a child’s neurodevelopment.
Is this a reason for certain couples to avoid having children?
No, not necessarily. The thing to keep in mind is that autism is an extraordinarily complex condition that’s probably influenced by hundreds of genetic, environmental, behavioral, and dietary factors, several of which may have to co-occur and reinforce one another for the condition to arise. So even though parental age is one of the most powerful variables, it probably accounts for 5 percent or less of any child’s total risk.
Do any other factors rise to this level of importance?
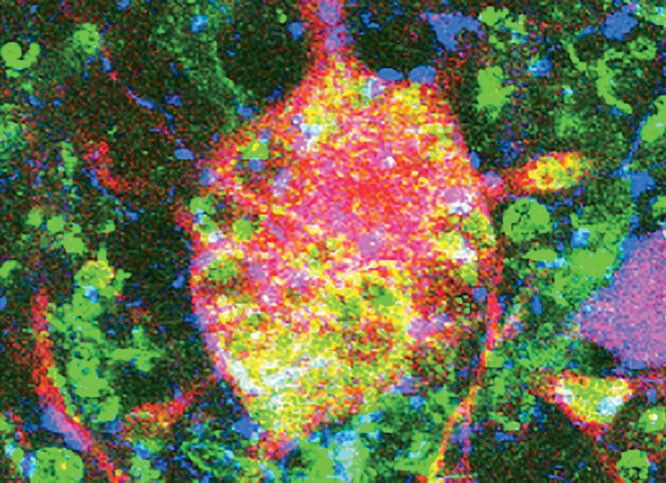
One of our more recent discoveries is quite significant: we found that if a pregnant woman experiences a high fever in her second trimester, her child’s chances of developing autism increase by 40 percent. We’re not sure why this is, but molecular evidence suggests that inflammation in the mother’s body may be associated with a delay in the formation of blood vessels in the fetal brain during a critical point in the development of the central nervous system.
Does it matter what causes the fever?
We suspect that any number of viral or bacterial infections can probably have this effect, but we’d need to conduct even larger studies to know for sure. Influenza appears to be implicated: the mothers of many of the children diagnosed with autism in our cohort suffered a serious bout of influenza in the second trimester. But the type of infection seems to be less important than its severity, since it’s the fever itself — indicative of a systemic, full-body inflammatory reaction — that we found to be strongly associated with autism.
That said, I wouldn’t want to be alarmist. A lot of women experience fevers while they’re pregnant and go on to have perfectly healthy kids. Again, the risk this poses for any particular child is quite small.
So what’s the takeaway for pregnant women or women who plan to get pregnant?
Get a flu shot. Get vaccinated against COVID-19. Wear a mask and practice social distancing. Keep your immune system strong by exercising and eating healthy food. And if you do get sick and have a high temperature, talk to your doctor about possibly taking an anti-inflammatory medication like ibuprofen. (Acetaminophen does not counter inflammation in the same way). Physicians have traditionally cautioned against taking ibuprofen while you’re pregnant because it carries a risk of miscarriage, especially in the first trimester, or possibly deformation of the baby’s heart if given close to the time of delivery, but administration of anti-inflammatory medications for fever during the second trimester might be discussed with one’s physician. At that stage, you really want to reduce a fever as quickly as possible.
Are any dietary factors important?
We analyzed the diets of all of the women and children who participated in our project to see if any vitamin or mineral deficiencies contribute to autism. What jumped out of the data was that women who take supplements of folic acid, or vitamin B9, early in their pregnancy are almost 40 percent less likely to have a child with autism. That wasn’t a shock because folic acid, which is found naturally in leafy vegetables, beans, and eggs, has long been known to be essential for fetal brain development. But our research revealed that folic acid supplements only protect a fetus against autism if a mother begins taking them shortly before conception and throughout the first two months of pregnancy, which is earlier than many women start on prenatal vitamins. That’s why I suggest that women who are planning a pregnancy talk to their doctors about taking prenatal supplements before they conceive.
We’ve also found preliminary evidence that heritable differences in how the body regulates levels of vitamin D in the body may be associated with autism in certain subsets of people with the condition, but we need to do additional research to confirm that.
Other researchers have claimed that altering an autistic child’s diet, such as by removing gluten, dairy, or other potential allergens, can sometimes ameliorate symptoms. Have you found any evidence that a child’s diet might contribute to the condition’s onset?
No, though it’s possible that dietary factors play such a role and that we’d just need larger studies with more statistical power to spot them. But we’ve tended to focus our investigations on pregnant women’s health in the Norway cohort because we believe that the roots of autism are likely established in the earliest stages of brain development, in the womb, and that improving our understanding of these processes holds promise for uncovering tractable pathways for prevention.
What are you looking at next?
Our findings about the role of fever in causing autism raise all sorts of questions. For example, we’d like to know if psychosocial stressors in the mother during pregnancy may pose a risk by triggering low-grade inflammation in the body that translates into neurodevelopmental risk for the child. The use of antidepressants by expectant mothers has previously been hypothesized as a risk factor for autism, but other data suggest that antidepressants themselves are unlikely to be the culprit; we’ve considered instead that underlying or untreated depression or anxiety may be the real danger.
Do you expect that we’ll see a spike in autism cases as a result of the COVID-19 pandemic?
Yes, sadly, I think that’s possible. And not just because many pregnant women have been getting COVID-19, but also because many people, pregnant women included, have been dealing with serious mental stress during the pandemic. It will be a few years before we know if autism rates rise in response, because the condition is usually diagnosed around age three or later. It is also quite likely that rates may rise more generally for a range of neurodevelopmental conditions, including ADHD.
Autism’s prevalence in the US has nearly tripled since 2000. Why?
Part of the explanation is certainly that doctors are more aware of the condition and are diagnosing it more frequently. But my colleagues and I suspect that other factors, like people having children later in life or environmental changes that are making our bodies more vulnerable to infections and immunological problems, are contributing to the uptick in cases.
You’ve spoken publicly about your own experiences raising a son with autism. Is there anything that you wish you’d known back when you were pregnant?
You know, it’s interesting, because I just discovered, through my own participation as a subject in an unrelated medical study, that I have a genetic mutation that’s known to interfere in the body’s absorption of folic acid. So this tells me that it’s possible I wasn’t getting enough folic acid when I was pregnant back in the late 1980s, even though I was taking the recommended four hundred micrograms per day. Now, did a lack of folic acid cause my son’s autism? That’s way too simplistic, because there were probably lots of genetic and environmental factors involved. Did it contribute? Maybe. I certainly wish that I’d known I was susceptible to folate deficiency when I was pregnant, because then I could have talked to my obstetrician about it and explored solutions.
What is the genetic variant you have? And are pregnant women routinely tested for it today?
The gene variant, which is carried by about 15 percent of all Americans, is located in the gene MTHFR. Pregnant women aren’t routinely tested for it, and a physician might initially balk at ordering it, unless he or she is knowledgeable of cutting-edge autism research and knows how to interpret its results. But if a woman can find a doctor who thinks the test is beneficial and she has good insurance, she might get it covered.
Are there any genomic tests that can tell an adult if he or she is likely to have a child with autism?
No, because the genetics of autism are still poorly understood. Although scientists have identified more than a hundred genes linked to the condition, we can’t say precisely what many of these genes do, nor the degree to which they increase an individual’s risk. There are some geneticists who will analyze and interpret men’s and women’s DNA in an attempt to estimate this risk. However, such analyses don’t offer definitive predictions, since we still haven’t identified all of the mutations involved in autism. Further, the influence of certain gene variants on autism may also depend on whether an individual is additionally exposed to specific environmental risks that may affect the function of that gene variant during key periods of early neural development — much as the rare inherited disorder phenylketonuria (PKU), caused by genetic mutations, can be treated by reducing or eliminating the amino acid phenylalanine from a child’s diet. A good source of information on this topic is the SPARK website of the Simons Foundation, a New York–based nonprofit that supports autism research.
Eventually, we’d like to get to the point where we’re able to recommend a whole range of preventive steps parents might take to mitigate the damaging effects of specific mutations they carry. But we still have a lot more work to do, both in terms of identifying the causes of autism and in understanding how various risk factors interact. Right now, we’re still building the scientific foundation for that kind of customized clinical care.
For more information on this research, see the following articles from Columbia's Mailman School of Public Health:
Study Identifies Biomarkers Linked to Autism Risk
Could Flu During Pregnancy Raise Risk for Autism?
Autism Risk Linked to Fever During Pregnancy
Autism Risk Linked to Herpes Infection During Pregnancy
This article appears in the Spring/Summer 2022 print edition of Columbia Magazine with the title "In search of autism's roots."