Every year, thousands of Americans die while awaiting a kidney transplant — a fate that’s usually blamed on a shortage of donated organs. But a new study by Columbia researchers reveals that many patients with chronic renal disease miss out on getting a donated kidney because transplant centers demand organs of unnecessarily high quality.
The study, led by Sumit Mohan, an associate professor of medicine and epidemiology at Columbia University Irving Medical Center, examined the histories of approximately twenty-six thousand patients who died while awaiting a kidney transplant between 2008 and 2015. It found that the vast majority of these patients had multiple opportunities to receive a transplant but that the available organs were declined by their transplant teams — typically without the patients’ knowledge — and subsequently given to people with less-critical needs. On average, the study found, each deceased patient’s team was offered sixteen kidneys that were deemed unsuitable.
“In 93 percent of these instances, the transplant teams cited concerns about ‘organ or donor quality’ in declining the offers,” says Mohan, who notes that few organs were rejected for being bad immunological matches. “Yet ultimately the kidneys were accepted for transplant in other patients.” (While Mohan and his coauthors were not able to track the outcomes of those subsequent transplants, they note that past research has shown that the number of times a kidney is declined does not affect a transplant’s chance of success.)
Mohan and his coauthors say part of the problem is that the US Centers for Medicare and Medicaid Services, which evaluates and publicly rates kidney-transplant centers, places too much emphasis on the fraction of transplants that each center executes successfully and too little on the number of patients served. Transplant centers are therefore rewarded for performing operations that they know will go smoothly and avoiding slightly riskier operations that, if performed more frequently, would save lives.
According to Mohan, whose paper appears in the online journal JAMA Network Open, the apparent risk aversion helps to explain why the US discards nearly 20 percent of all donated kidneys — a much higher rate than other countries.
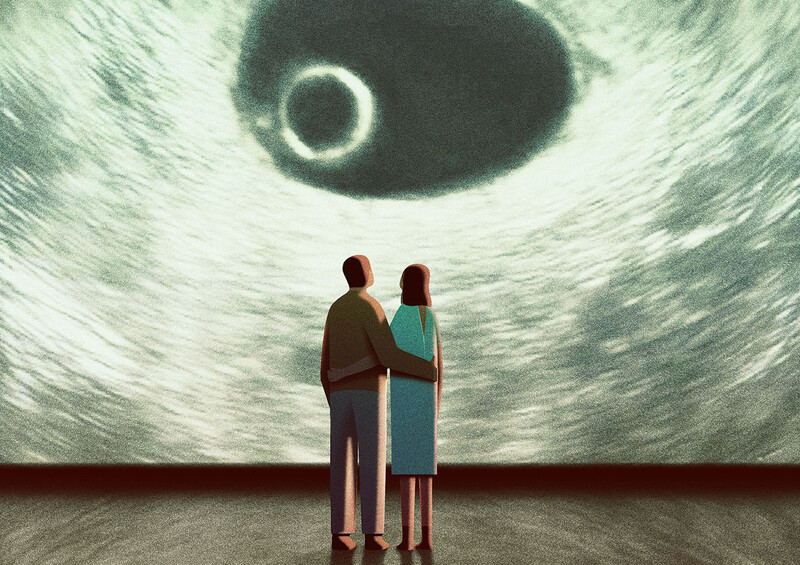
To make the US transplant system more efficient, Mohan and his colleagues recommend that the Centers for Medicare and Medicaid Services update its evaluation and rating system. They also suggest that better communication between patients and transplant centers is needed. Currently, Mohan says, transplant centers don’t ask patients how selective they want their physicians to be when scrutinizing available kidneys, nor do they typically disclose to patients when organs are declined, or why.
“Physicians must act quickly when deciding whether to accept particular organs, so they cannot consult with patients in real time,” he says. “However, there’s no reason doctors can’t discuss in advance how cautious or aggressive patients want their transplant team to be in making these decisions. Does a patient want to accept the next available kidney? Or does she prefer to hold out for an organ from a young, healthy donor? A patient should have a say in that.”
Giving patients the option of instructing doctors to use a more liberal standard in accepting kidneys poses few risks, Mohan insists, because all donated kidneys taken into the nation’s organ-allocation system are of relatively high quality.
“The bottom line is that it’s often better to get a less-than-perfect kidney sooner than to wait for the perfect kidney to come along,” he says.