A woman who tells her doctor that she has a family history of breast cancer and identifies herself as an Ashkenazi Jew likely will be referred for a genetic test. And why not? The screening is cheap and effective, as geneticists have identified specific mutations common among Ashkenazi women that cause breast cancer.
That’s how genetic information ought to inform healthcare delivery, right? The only problem, says Sheila Rothman, a professor of public health, is that few people benefit from this kind of group-specific knowledge. In a salty paper published in the November 2006 issue of The American Journal of Public Health, Rothman points out that although Ashkenazi women commonly are perceived to be at risk of breast cancer, they don’t have higher incidences of the disease than do women of other ethnicities. Geneticists simply know more about the susceptibility of some Ashkenazim. For that, credit serendipity: Researchers have access to large repositories of genetic samples used during decades of studies on the link between Ashkenazi ethnicity and Tay-Sachs disease.
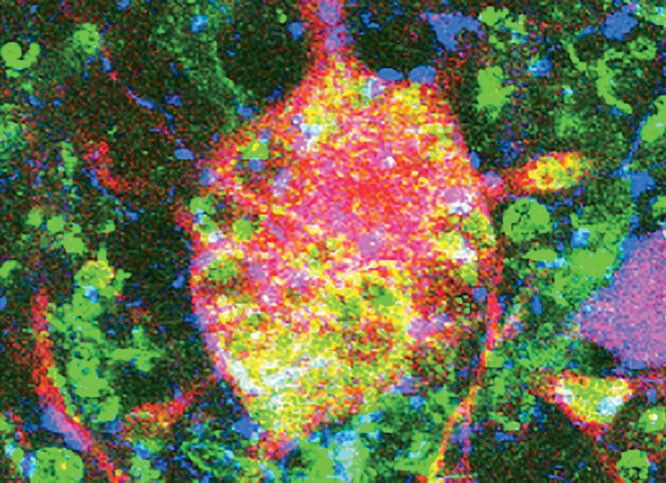
In the 1990s, geneticists noticed that 2.5 percent of Ashkenazi women have one of three mutations among many known to cause breast cancer. “That’s a high prevalence for those three specific mutations,” says Rothman, “but what is the prevalence of mutations that cause breast cancer in other groups of women? We don’t have that kind of information yet, and that’s led to a disparity in care.”
While an Ashkenazi woman can be screened for relevant mutations for about $400, for instance, screening a non-Ashkenazi Jewish woman for all the mutations known to cause the disease costs about $3000. As a result, Ashkenazi women with a family history of breast cancer are more than twice as likely to undergo genetic testing as are other women at similar risk.
Rothman says that the medical profession must address the “serious scientific and social concerns” raised by genetic research that targets racial and ethnic groups. In the case of breast cancer, she says, medical panels should be formed to guide research aimed at identifying the genetic susceptibility for the disease among other ethnic groups. Rothman points out that recent genetic-research surveys — including among Spanish, German, Dutch, Polish, and Hispanic women — have found a high prevalence of the so-called “ancestral Jewish mutations” in other groups.
"Doctors and geneticists should be identifying all women who are at risk for the disease," she says, "and making sure they have similar access to screening."
Rothman, whose work is funded by the National Institutes of Health's Centers for Excellence in Ethical, Legal, and Social Implications Research, currently is studying how Ashkenazi women are affected by the perception that they are prone to developing breast cancer. "There is a concern among some Jewish communities that it has caused stigmatization," she says. "We're going to examine how their being linked with this disease affects the group identity, and what kind of political and social actions that leads them to, such as on issues regarding the privacy of genetic information."