In late January, when most Americans were hearing about the novel coronavirus for the first time, the Columbia epidemiologist W. Ian Lipkin was in Beijing, advising the Chinese government on its response. One of the world’s leading virus hunters, Lipkin has nearly four decades of experience in identifying, tracking, and developing diagnostics for emerging infectious diseases. He frequently travels to other countries to help them fight epidemics, as he did for China with SARS in 2003 and for Saudi Arabia with MERS in 2012. This past winter, he booked a flight to Beijing immediately upon learning from Chinese colleagues that the virus was spreading quickly.
“At that point, it’s a race against time,” he says, “because until you have a vaccine or treatment, containment is your only hope.”
After meeting with health and science ministers, fellow epidemiologists, and physicians working on the front lines, Lipkin delivered a series of recommendations to senior Chinese leaders. He endorsed their efforts to lock down Wuhan, urged them to close hundreds of live-animal markets like the one at the center of the outbreak, and advised them to reveal everything they knew about the virus to the international community. “‘Not only will this benefit global health,’ I told them, ‘but it will demonstrate to the world that you’re a reliable and transparent partner,’” Lipkin says.
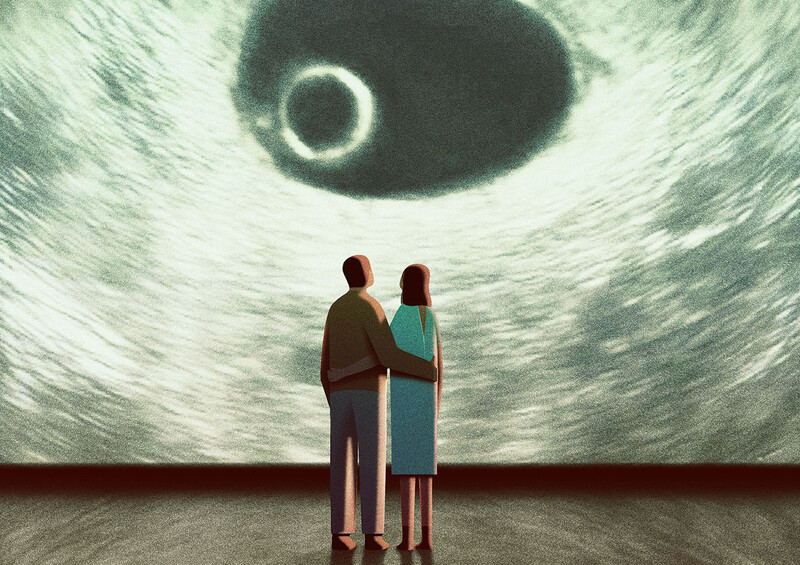
Meanwhile, back in New York City, Lipkin’s team at the Mailman School’s Center for Infection and Immunity was already working on an ultrasensitive test for COVID-19, one capable of detecting small amounts of virus that conventional types of diagnostic tools might miss. (Some team members flew with Lipkin to China to study a sample of live virus as a reference.) Such a technology would be invaluable, Lipkin knew, if people carrying light viral loads, and possibly exhibiting no symptoms, were nevertheless contagious.
By March it was apparent that Lipkin’s instinct had been right: large numbers of people unaware they were infected with COVID-19 had contributed to the spread of the disease. In fact, one of the first comprehensive analyses of transmission patterns — published by Columbia data scientists Jeffrey Shaman ’03GSAS and Wan Yang in the journal Science that month — found that asymptomatic people were driving two-thirds of the disease’s spread.
As this magazine went to press, Lipkin was himself recovering from COVID-19, which he contracted through routine social exposure in New York City. The illness barely slowed him down, though: by April, he and his colleagues had completed work on their diagnostic system, which also identifies people who have recovered from COVID-19 and whose blood plasma or antibodies might be useful in producing new medications. They hope to soon roll out what they call their C3 test, which has been approved by the FDA, as part of community screening programs in the US and abroad.
But Lipkin is also looking further out on the horizon, with an eye toward averting future pandemics. The only way to contain a highly contagious new disease in our globalized world, he says, is to spot it quickly and immediately bring the full power of the international scientific community to bear in identifying the guilty pathogen and determining how it is being transmitted. To ensure that this happens in a timely manner, Lipkin says, wealthy nations must devote more resources to disease-detection systems both within their borders and in developing countries.
Lipkin, in conjunction with epidemiologists in more than a dozen countries, is developing plans for such a surveillance system. Called the Global Infectious Disease Epidemiology Network, or GIDEoN, it would equip scientists in parts of Africa, Southeast Asia, and South America with advanced biomolecular tools that Lipkin and his Columbia colleagues have designed for rapidly identifying novel pathogens. Participating researchers would be able to share their observations automatically with other GIDEoN scientists around the world in real time.
“So the moment anybody in the network sees something suspicious, everybody sees it,” says Lipkin, who is currently trying to raise private funding for the effort. “You could think of it as an international immune system.”
He says that GIDEoN would complement existing surveillance networks, such as one run by the World Health Organization. That system, he says, is hampered both by a lack of on-the-ground diagnostics in many countries and by a dependence on national governments to voluntarily report outbreaks. Many countries have been suspected of delaying reports of past outbreaks, Lipkin notes, for fear of having limitations placed on their agricultural exports, travel, or tourism.
“Our network, because it would be run by scientists and public-health practitioners, would take a lot of the politics out of the equation,” Lipkin says.
This article appears in the Spring/Summer 2020 print edition of Columbia Magazine as part of the cover story, "What We Have Learned From the Pandemic (So Far)."