Pandemic Highlights Urgent Need for Long-Term Vaccine Development
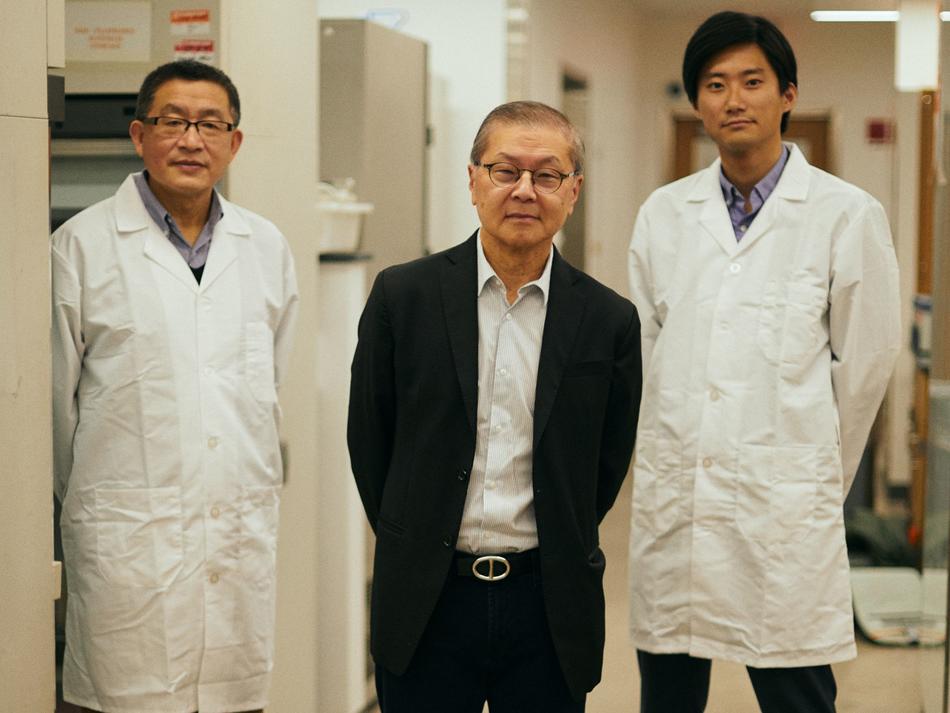
David D. Ho ’00HON, the world-renowned AIDS researcher, had just started to settle into his laboratory at Columbia University Irving Medical Center when news broke of a novel coronavirus spreading across China. He and his team of twenty-five scientists at the Aaron Diamond AIDS Research Center (ADARC) — a prestigious organization that Ho has led since 1991 and that became a part of Columbia’s medical school in late 2019 — quickly shifted gears. The center’s ongoing efforts to improve HIV treatments and find a cure for AIDS, Ho decided, would temporarily be scaled back so that he and his colleagues could devote most of their energies to developing drugs to treat COVID-19.
“In the past we’ve stepped in to help fight other viruses, such as SARS, bird flu, and Ebola, but we knew that our involvement here was going to be on another level,” says Ho, who in addition to directing ADARC is the Clyde ’56 and Helen Wu Professor of Medicine at Columbia. “This was going to be all hands on deck.”
ADARC, which occupies two floors of laboratory space in the medical campus’s Hammer Health Sciences Center, is at the center of Columbia’s ambitious multipronged effort to study COVID-19 and related coronaviruses. The program, which is supported by more than $10 million in private donations, involves not only ADARC scientists but members of several other Columbia research teams that have experience in developing antiviral therapies against either HIV or hepatitis.
“Viruses tend to share some basic characteristics, so an approach that works against one virus is often a good starting point for fighting another,” says Ho, a pioneer of combination antiretroviral therapy for AIDS, a treatment approach that has dramatically extended patients’ lives through the simultaneous administration of multiple drugs at the first sign of infection.
In many ways, the research is similar to other COVID-19 drug-discovery programs now underway at laboratories around the world. Ho and his collaborators are genetically analyzing the new coronavirus for clues about how it might be susceptible to drugs and then screening chemical compounds that they think might be able to incapacitate it. The Columbia scientists, like others, are proceeding at a breakneck pace, employing an array of experimental new technologies that are designed to reduce the amount of time this work takes.
“We’re trying to condense the initial stages of drug discovery, which would ordinarily take several years, into just a few months,” says Ho. He expects to bring a number of vaccine and drug candidates to clinical trials within a year.
But the Columbia initiative is different from others in one important respect: it is aiming to develop therapies that will work not only against the coronavirus that causes COVID-19 but against the wide variety of coronaviruses that could infect people in the future. A diverse group of microbes most frequently found in bats, pigs, birds, and other animal hosts, coronaviruses have in several cases jumped into humans and caused outbreaks of serious disease (four other human coronaviruses cause milder, cold-like illness). These outbreaks have happened three times so far this century — with severe acute respiratory syndrome, or SARS, in 2003; Middle East respiratory syndrome, or MERS, in 2012; and now COVID-19 — and Ho believes that additional coronavirus “spillover” events are destined to occur.
“So while we’re undertaking this effort with a great sense of urgency because of the nature of the current outbreak, we’re also thinking ahead to what we may confront in the future and trying to come up with more permanent solutions,” he says.
To do this work, Ho and his collaborators — who include Columbia faculty members Alejandro Chavez, an assistant professor of pathology and cell biology; Stephen P. Goff, the Higgins Professor of Biochemistry and Molecular Biophysics and a professor of microbiology and immunology; Jingyue Ju, the Samuel Ruben–Peter G. Viele Professor of Engineering; and Yosef Sabo, an assistant professor of clinical medical sciences — are making lists of essential features of the COVID-19 coronavirus that could be targeted with drugs and then looking to see which of those features are also present in other coronaviruses. The scientists will use a new drug-screening technology developed by Chavez to test promising compounds against dozens of strains at once. The technology represents a radical improvement over traditional drug-screening tools, which limit scientists to observing the effects of drug candidates on a single virus at a time.
If Ho and his colleagues are able to create a therapy that one day proves effective against a never-before-seen illness, it will be a first. Nobody has ever developed a treatment for a viral disease that didn’t exist yet. But Ho says that if recent history is any guide, emerging diseases will continue to crop up with regularity, forcing health officials to scramble to contain outbreaks while scientists frantically search for vaccines and treatments — which may come months or years later, if at all. A more forward-looking drug-development strategy could ultimately save lives and money, says Ho.
“What’s happened in the past when new infectious diseases have emerged is there is an initial surge of financial support for creating drugs, but then, once the outbreaks are brought under control, support for the research begins to dry up,” he says.
Ho notes that in 2003, at the height of the SARS epidemic, his laboratory and several others were close to developing treatments. Once the epidemic was contained, though, grant support disappeared and critical work was left unfinished. Ho now regards that venture as a lost opportunity, because the strain of coronavirus that caused SARS is extremely similar to the one that causes COVID-19 — so similar, in fact, that he thinks the treatments his team had started to develop for SARS may very well have protected people against the new disease.
“At the very least, I think we’d be closer to having a treatment for COVID-19 now if we’d have been able to continue the work,” he says.
Given the magnitude of the current pandemic, Ho says that he is cautiously optimistic that governments and private donors will continue to support research on other strains of coronavirus once the outbreak subsides.
“Now it’s the third time we’ve been through this,” he says. “I doubt that the world’s going to drop the ball on this one.”
This article appears in the Spring/Summer 2020 print edition of Columbia Magazine as part of the cover story, "What We Have Learned From the Pandemic (So Far)."