Hal the robot boy doesn’t sound good. He is wheezing, coughing, and gasping for air, and when a young woman approaches his bed, he calls out feebly for his mother.
“You don’t need to be scared,” says the nursing student, Terri Phan.
“But I can’t breathe,” Hal groans, eking out a staccato computerized sob.
“We’re going to help you with that, don’t worry,” another student, Erin Pratt, assures him.
Glancing down at Hal’s hospital intake form, Phan and Pratt read that he is a six-year-old asthmatic who has been admitted to the hospital after struggling to breathe for nearly two days. They quickly come up with a plan: they will give him oxygen, check his vital signs, make sure that he gets x-rays and blood tests to determine if he’s suffering from a respiratory infection, and administer a medication to open up his airways. In the meantime, they will continue to speak soothingly, hoping to ease his anxiety. It’s exactly what they’ve been taught to do.
They know all the protocols, but what no one could have prepared them for is how difficult nursing can be when a child is crying, complaining, and peppering you with questions the whole time.
“What is that?” Hal asks at one point, when he sees Phan coming toward him with an air mask.
“It’s just oxygen to make you feel better,” she whispers.
“What’s oxygen?”
“It’s in the air we breathe.”
“But I don’t even want to be here anymore!” he protests, squirming to avoid her touch. He’s unhappy, and he’s not going to make this easy.
A few years ago, aspiring nurses or physicians would have had to wait until their clinical rotations to have an experience as intense as this. Today, however, with the availability of highly realistic medical training robots like Hal — whose silicone body mimics a wide variety of disease symptoms and can be hooked up to medical monitoring equipment — even first-semester students are able to hone their skills in simulated hospital settings.
“It’s one thing to read about asthma in a textbook and quite another to treat someone who is frightened and confused,” says Annie Chan ’15NRS, a licensed nurse practitioner who, on a recent Friday afternoon, was controlling Hal from behind a one-way mirror in a mock examination room at the simulation center. “We’re helping students bridge that gap, from the very first month they arrive here.”
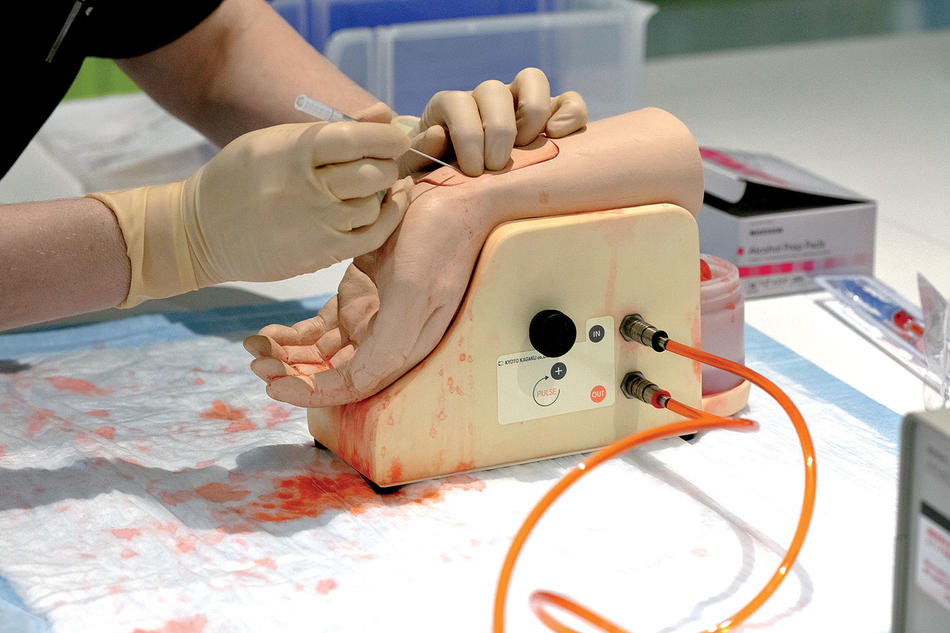
For decades, nursing and medical students have used simple plastic manikins to practice inserting needles, suturing wounds, and administering CPR. But with a new generation of advanced medical robots now on the market, teaching hospitals are increasingly running simulation exercises to immerse students in high-pressure situations where they must think critically and make complex decisions in real time.
“When I was a student, back in the 1990s, our manikins didn’t do much,” says Kellie Bryant, an assistant professor of nursing who directs the simulation center. “They weren’t particularly realistic, and they certainly weren’t interactive. Now we have robots that cry, bleed, breathe, blink, urinate, respond to medications, talk back to you, and make all sorts of facial expressions — it’s eerily similar to treating a real person.”
Columbia Nursing’s sixteen-thousand-square-foot Helene Fuld Health Trust Simulation Center, which occupies two whole floors of a new seven-story building on the University’s medical campus in Washington Heights, is one of the largest and most advanced of its kind. It features fourteen mock hospital rooms, each furnished with all the equipment one would find in a real clinical setting: blood-pressure cuffs, thermometers, instruments for checking eyes and ears, oxygen supplies, disinfectants, EKG monitors, and laptop computers for maintaining electronic health records. Synthetic body parts abound, for practicing skills like drawing spinal fluid, performing tracheotomies, and inserting urinary catheters. And then there are the state-of-the-art robots. In addition to Hal, there is a female robot that delivers a baby and is prone to myriad postpartum complications, an infant robot that suffers everything from low blood sugar to respiratory distress, and an adult robot that is designed specifically to be sedated and anesthetized for surgery. These marvels of computer and mechanical engineering, built by companies like Gaumard Scientific, CAE Healthcare, and Laerdal Medical, can cost anywhere from $40,000 to $220,000.
The simulation exercises that take place at Columbia Nursing are run by faculty instructors who, in addition to manipulating the robots’ vital signs and movements, can control their speech by talking into a computer that alters their voice. They record their students’ performance on video so that they can later review and critique it.
“You can throw all sorts of complications into a scenario by tweaking a robot’s pulse, respiration rate, and other vitals as you go,” says Bryant. “It’s incredibly dynamic.”
The exercises often incorporate role-playing, as teaching assistants take turns pretending to be patients’ family members. This can add a messy interpersonal dimension to what is already a tense situation; one team of students was recently evaluated for their response to overhearing Hal’s parents discuss who should step out to buy cigarettes.
“So the challenge there is: how do you talk to them about smoke being a trigger for asthma without undermining them in front of their child or making them feel judged?” says Bryant. “At the same time, the students are still juggling a million clinical things happening. It’s a lot to handle.”
The advantage of simulation training, educators say, is that it provides a safe place for students to make mistakes, ask questions, and reflect on their strengths and weaknesses. They note that in the past, when young nurses and doctors learned most of their clinical skills during a residency, they tended to downplay the gaps in their knowledge for fear of frightening patients or being blamed for medical errors that might occur. In a mock examination room, on the other hand, the worst thing that can happen when a robot gets a botched IV line, urine catheter, or tracheotomy is that it has to have one of its replaceable body parts swapped out before the next student takes a crack.
“I tell my students that whatever happens in the simulation center stays in the simulation center — it’s Vegas rules,” says Chan. “We embrace the mistakes, because every mistake that happens in this place is one that probably won’t be committed by that student again.”
Bryant says that simulation training became popular in medical and nursing schools after 1999, when a report by the Institute of Medicine (now the National Academy of Medicine) revealed that medical errors are a leading cause of death in the US. Since then, research has shown that medical simulation can improve patient safety.
“One study found that when nurses and doctors used simulation exercises to practice treating children who experience cardiac arrest, survival rates for the condition increased from 33 percent to nearly 50 percent,” Bryant says.
For students, the benefits of simulation can be summed up in one word: experience. “There are so many aspects of this work that you can’t learn in a classroom,” says Katie Chen, a master’s degree student. “Like, how do you translate medical terminology into everyday language without sounding patronizing? How do you communicate with someone who’s fading in and out of consciousness? How do you efficiently update other nurses about a patient’s condition when your shift ends? It’s just practice, practice, practice.”
And when a student has mastered one challenge, Hal the robot boy is ready with another. Next time he could be suffering from anaphylactic shock, appendicitis, or any of dozens of other conditions. He always makes a full recovery. Just don’t expect him to be a model patient.