Every year, millions of people in the developing world die of syphilis, tetanus, hepatitis, and other infections that could be easily treated with antibiotics. Often, the problem is not a lack of medicine but a failure to diagnose patients. That’s because health workers don’t have a practical way to screen people in rural areas: they must collect blood samples in remote health clinics, transport the samples to a laboratory that may be hundreds of miles away, and then return weeks later in an attempt to locate everybody who tested positive.
“This is time-consuming and very expensive,” says Samuel Sia, a Columbia associate professor of biomedical engineering. “Aid agencies literally don’t have the resources to do it.”
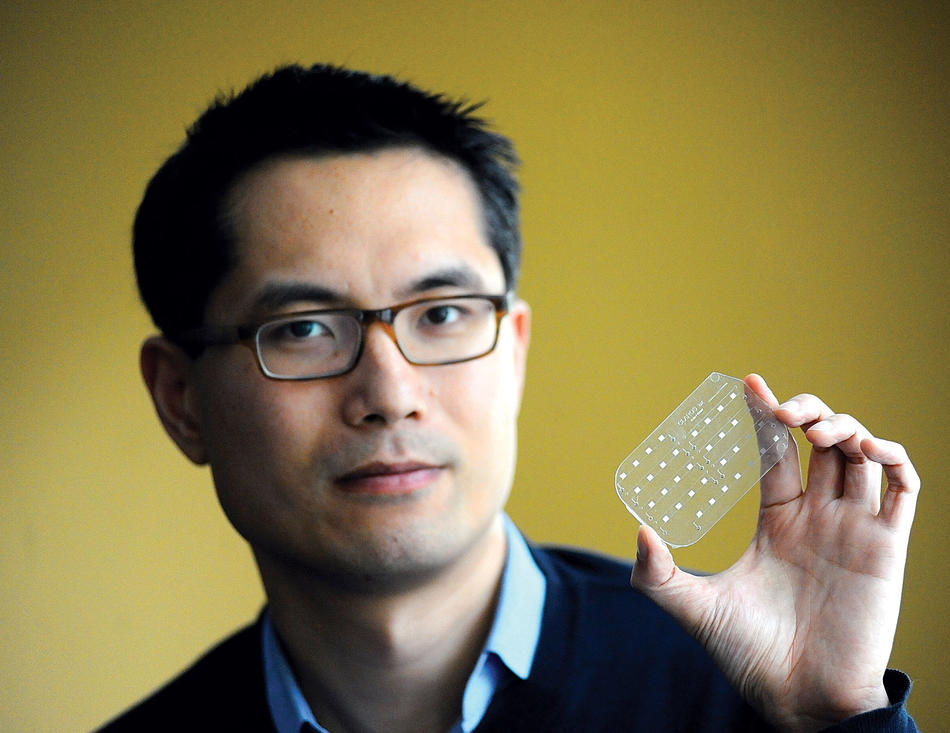
Sia recognized this problem while traveling in Togo as a graduate student about ten years ago. And he believes that he has a solution: a portable diagnostic tool the size and shape of a credit card. The device, which he calls an mChip, requires just a drop of blood from a finger prick and reveals its diagnosis in fifteen minutes.
“This could dramatically reduce the cost of a large-scale screening program,” Sia says. “It could also improve the likelihood that a sick person will get treated, because health workers could administer medicine on the spot.”
In creating the mChip, Sia’s research team had to miniaturize and tweak many aspects of the diagnostic process. A special anticoagulant is used to get blood flowing through the mChip’s hairline channels; ultimately, tiny gold particles react to form a cloud of silver ions when there is sign of an infection.
“If you see silver, you’ve got a positive diagnosis,” says Sia. “It’s as easy as reading a home pregnancy test. With conventional diagnostics, you need a microscope to view the chemical reaction that is the basis of your test.”
The mChip is not the first portable diagnostic device of its type; handheld tools already exist for detecting HIV. But the mChip has an advantage over similar technologies, Sia says, in that it is a versatile tool that could be easily adapted for testing for hepatitis, herpes, gonorrhea, and chlamydia, as well as HIV and syphilis.
Over the past four years, Sia and several collaborators, including Wafaa El-Sadr, a Columbia public-health professor and a prominent HIV/AIDS researcher, have been using the mChip on a trial basis in Rwanda. They recently published a paper in Nature Medicine reporting that it detects HIV and syphilis with nearly 100 percent accuracy. This was based on a small study of a few hundred people; Sia and a private company he co-founded in 2004, Claros Diagnostics, are now seeking funds to conduct larger clinical trials.
“One of the most important applications for the mChip is for screening pregnant women and infants, because deadly infections can get passed on to newborns,” Sia says. “In rural areas, drugs are often available to treat these infections, but you don’t know whom to give the medicine to. So the main challenge is really diagnostics.”