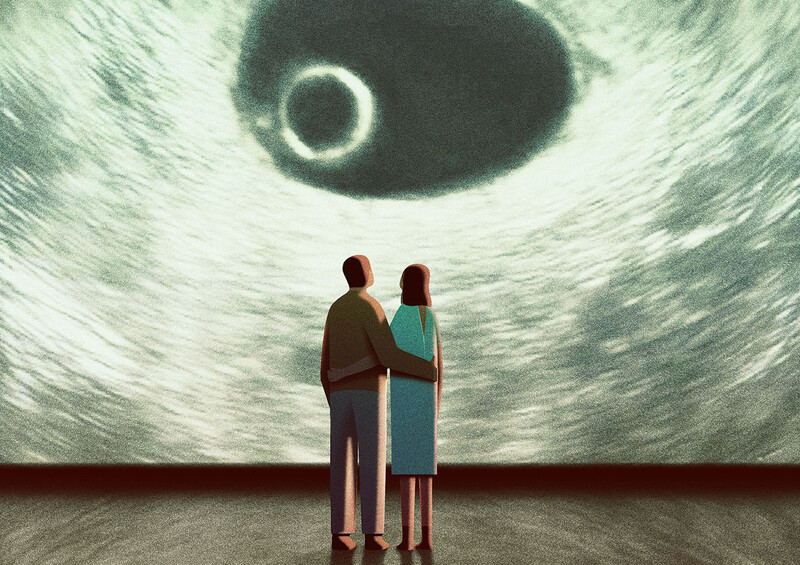
When Lia McCabe was 25 and working as a financial-planning assistant in Manhattan, she started having excruciating headaches and joint pain so intense that she couldn’t walk or even hold a pen. She was making stupid mistakes, like slamming drawers on her hand and opening cabinets on her head. And then there were the memory problems: She knew she had to stop working the day she showed up and couldn’t find her desk.
By the time she was tested for Lyme disease two years later, McCabe was bedridden and severely mentally impaired. “I couldn’t add two plus two,” she says. “At my worst, I didn’t recognize my parents.”
McCabe tested positive for Lyme disease, a tick-borne bacterial illness that’s difficult to diagnose, in 1994. She’s since learned to walk again and to manage her pain by taking lots of powerful intravenous antibiotics. Her cognitive ability has improved, too, although she still can’t hold a job. While running errands in her own neighborhood, in fact, she carries a map in case she gets lost.
“I begin every morning with a game of solitaire to see how I’m doing,” she says. “I don’t want to pay bills or make a big decision on one of my bad days.”
Like McCabe, thousands of Americans today suffer serious physical and neurological problems despite having been treated for Lyme disease. Scientists can’t agree on what makes them sick. Is the Lyme bug still in their systems? Did the initial illness simply wreck their bodies? Or do they actually have some other condition with similar symptoms? Debate about whether to give them more antibiotics is contentious among scientists and confusing to patients; the Infectious Diseases Society of America (IDSA) weighed in on the matter last October, publishing strict new diagnostic guidelines that essentially deny that chronic forms of Lyme disease exist.
But a group of Columbia professors led by Brian Fallon, a clinical psychiatrist whose own research cuts across the boundaries of medicine and neurology, won’t concede that point. In April, Columbia University Medical Center (CUMC) launched the first research center in the world to focus on chronic health problems associated with Lyme disease. Supported in part by $3 million in gifts from the patient-advocacy groups Time for Lyme and the Lyme Disease Association, Columbia’s new Lyme and Tick-Borne Diseases Research Center is investigating the basic science of chronic Lyme disease in hopes of developing new diagnostic tools and more effective treatments.
“I’ve seen too many healthy people get Lyme disease and then never be the same again,” says Fallon ’85PH, ’85PS, who directs the new center. “I know that chronic Lyme disease is real. But what exactly is it, and how do you treat it? Nobody knows because few researchers have asked these questions.”
Doctors Divided
Lyme is one of the fastest-spreading infectious diseases in the United States, according to the Centers for Disease Control and Prevention, with roughly 23,300 new cases reported in 2005, up 22 percent from 2001.
The illness is carried by deer ticks in the Northeast, where 90 percent of all U.S. cases are reported, and by Western black-legged ticks on the West Coast. Lyme has become more prevalent since its discovery in 1975, scientists say, partly because suburban neighborhoods have expanded into wooded areas where the ticks thrive. “In parts of East Suffolk, Long Island, and Fairfield County, Connecticut, it’s a tick haven,” says Rafal Tokarz, a Columbia microbiologist and postdoctoral researcher who studies ticks. “People walk out in the backyard with their dogs, and they come back in with literally four or five ticks on them."
A person with an infected tick burrowed in her skin for longer than 24 hours is at high risk for contracting Lyme. If she gets the disease, a large red rash typically appears, accompanied by flulike symptoms within a couple of weeks. The telltale bull’s eye–shaped rash doesn’t show up in about 40 percent of all Lyme cases, however, and early symptoms such as fatigue, fever, headaches, and achy joints can mean just about anything. To further befuddle doctors, there’s this: Blood tests cannot rule out Lyme because the bacterium that causes it, Borrelia burgdorferi, enters the body in such small amounts.
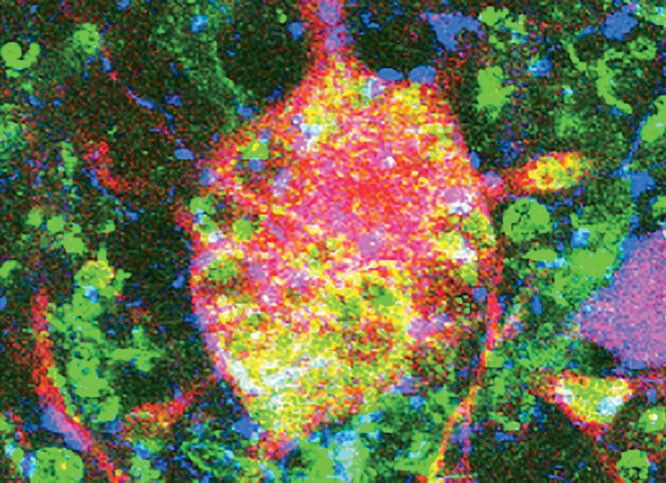
Physicians may mistake the disease for everything from chronic fatigue to the ordinary flu, according to Fallon. And that’s when the real trouble starts, because if treatment is delayed by even a few days, B. burgdorferi can spread throughout the body, causing inflammation in the joints, the spinal column, and major organs. The corkscrew-shaped bug is especially adept at invading the nervous system, Fallon says, leading to mood disorders and memory problems in 10 to 30 percent of patients who aren’t treated promptly, and in 5 percent who are. In more rare cases, he says, Lyme causes manic depression, seizures, numbness in the hands and feet, speech problems, and even dementia.
How effective is treatment? That’s another question that divides the medical community. Most Lyme experts insist that a single four-week course of antibiotics cures the disease, even when it was detected late. Citing two major studies in 2004 that didn’t find any B. burgdorferi in people once treated for Lyme, these experts say that if health problems persist it’s likely that the patient contracted a new, unrelated illness. The majority of Lyme researchers therefore oppose administering more antibiotics, which carry a risk of allergic reaction or life-threatening staph infection when delivered by catheter. The IDSA’s new guidelines for diagnosing Lyme disease reflect this perspective, calling for antibiotic treatment only when a rash appears or when blood tests reveal an active infection. The American Academy of Neurology (AAN) published similar standards this spring.
“We don’t deny that people who say they have chronic Lyme disease are suffering,” says IDSA spokesman Steven Baragona. “But it’s not clear that what they’re suffering from is Lyme disease.”
Fallon, on the other hand, is among a smaller number of scientists who believe that B. burgdorferi, like the syphilis bacterium it closely resembles, lies dormant within human cells, where medications have trouble attacking it. “That’s been demonstrated in vitro,” he says, “but not yet in the human body.” Fallon is about to publish a study suggesting that repeated courses of antibiotics relieve certain symptoms of chronic Lyme; the research provides a counterpoint to previous studies that found no such benefit. It’s also possible, Fallon says, that the initial B. burgdorferi infection triggers an autoimmune response, prompting the body to continually attack itself, and that the bug causes permanent tissue damage.
“There’s probably a complex combination of factors at work,” says Fallon, 51, who is an associate professor. “We want to learn how these mechanisms operate in different patients, so we can tell who’ll benefit from more antibiotics and who should be treated instead for individual symptoms like pain or depression. Right now, doctors and patients are frustrated because everything about Lyme disease seems so ambiguous.”
Advocating Caution
In 1994, when Fallon launched Columbia’s first Lyme research unit, little was known about the psychiatric effects of the disease. Fallon was among the first to describe them. In one study, he found that Lyme patients are two to three times more likely to develop depression than people with similarly debilitating conditions, such as lupus and rheumatoid arthritis. Then, in 2001, Columbia psychologist Felice Tager showed that children with a history of Lyme are prone to cognitive problems.
These Columbia studies had a profound impact. Physicians previously knew that Lyme causes arthritis and a handful of neurological conditions like meningitis and cranial nerve palsies, but thanks to Fallon and his colleagues they gradually came to recognize that the disease can bring about a wide range of psychiatric problems. As a result, many infectious disease experts actually worry that doctors are now overdiagnosing Lyme and needlessly prescribing antibiotics. “There’s been so much publicity around Lyme disease, I think that clinicians today are more likely to accept the possibility that Lyme patients have a persistent infection than is warranted by the research,” says Eugene Shapiro, a Yale professor of pediatrics who coauthored the IDSA guidelines.
Fallon, who agrees that diagnostics must be made more precise, advocates a cautious approach to clinical work. Doctors should consider a diagnosis of chronic Lyme most seriously, he says, when clusters of symptoms appear and only after patients have tried standard treatments for their individual symptoms. Yet he insists that doctors still aren’t sensitive enough to Lyme’s broad symptomatology. Surveys have shown, for instance, that many physicians mistakenly believe that patients cannot have middle- or late-stage Lyme if they don’t have arthritis. In fact, arthritic symptoms are typically supplanted by cognitive problems one to two years after a patient contracts Lyme disease, Fallon says.
To make diagnosis more scientific, researchers at Columbia’s new Lyme center are trying to identify biomarkers, bodily characteristics that signal the disease’s presence. In a forthcoming paper coauthored with Fallon, Columbia brain imaging experts led by radiologist Ronald Van Heertum, neuropsychologist Harold Sackeim ’72CC, and mathematician James Moeller identify a specific region of the brain in which blood flow appears to be altered by B. burgdorferi. “This research eventually might tell us whether the Lyme bacteria have invaded the central nervous system,” Fallon says, “and therefore whether to risk giving patients the powerful IV antibiotics that are designed to reach nerve cells.”
Fallon and his colleagues recently completed another study that suggests repeated courses of the IV antibiotic Ceftriaxone provide long-term benefits in physical functioning but only short-term cognitive improvement to chronic Lyme patients. The researchers also are investigating the genetic basis of Lyme disease. If they can explain why some people are less effective at fighting the Lyme infection or why their immune systems produce an overly intense inflammatory response, Fallon says, it could open up new treatment possibilities.
Faulty Guidelines?
The neurologist Andrew Pachner once called Lyme disease the “new great imitator,” updating an old epithet for syphilis, which mimics other illnesses when left untreated and was difficult to diagnose prior to the 1930s. Like syphilis back then, Lyme disease today is often derided as a “wastebasket diagnosis,” a too-easy explanation for otherwise mysterious ailments. Amongst physicians, the Lyme debate can get personal: Doctors who specialize in treating chronic Lyme have even been accused of exploiting desperate patients.
In order to discourage careless Lyme diagnoses, the Maryland state legislature considered a bill this spring that would have written into law the IDSA’s and AAN’s new diagnosis and treatment guidelines, which are nonlegally binding ethics standards. The proposed legislation died in the state Senate. Around the same time, several state medical boards disciplined doctors who give chronic Lyme patients repeated courses of IV antibiotics.
Time for Lyme and the Lyme Disease Association, the influential patient-advocacy groups that funded Columbia’s new center, are lobbying hard against the new IDSA and AAN guidelines, which, they say, leave chronic Lyme patients without any realistic treatment options. Their case is being heard in some quarters: Connecticut Attorney General Richard Blumenthal now is investigating whether scientists who wrote the new guidelines ignored evidence they didn’t like. Among Blumenthal’s stated concerns is that insurance companies will use the guidelines to deny coverage of doctor-prescribed treatments.
Physicians at Columbia’s Lyme center don’t have to worry about being censured because they administer antibiotics only as part of approved research studies. But Fallon still refers chronic Lyme patients to doctors who prescribe IV antibiotics. “I’m not fixated on using repeated courses of antibiotics,” he says, “but I do believe the option should be left open for doctors to consider.”
As to the underlying scientific debate, Fallon takes a philosophical view: Both the physicians who treat chronic Lyme with additional antibiotics and the doctors who oppose that approach, he says, are practicing medicine “in a reasonable fashion” based on a clear set of diagnostic principles. It’s just that they can’t agree on what the principles ought to be. Do the health consequences of chronic Lyme disease outweigh the risks of antibiotic therapy? Or should doctors adhere to narrow clinical criteria of Lyme, and therefore risk leaving some patients untreated?
“Part of what makes Lyme disease devastating is that there’s so much confusion in the medical community,” Fallon says. “Now we have two prominent medical organizations saying that the question about antibiotics is closed, but I don’t think it’s closed. We still don’t know what causes chronic Lyme, and evidence suggests that more antibiotics might help some people. At Columbia, we’re trying to keep these questions open.”