It is the closest scientists have ever come to cloning human cells as a means of developing medical treatments.
On October 5, researchers at the New York Stem Cell Foundation (NYSCF) and Columbia University Medical Center (CUMC) reported in the journal Nature that they have discovered a new way to create embryonic stem cells that contain a sick person’s unique DNA.
Their breakthrough is considered significant because scientists have long sought to develop patient-specific embryonic stem cells as a way to grow replacement tissue for people with heart disease, Parkinson’s, and other illnesses. But no method has ever proven safe and useful.
The scientists at NYSCF and Columbia put a new twist on an old cell-replacement strategy. They started by extracting nuclei from skin cells of people with type 1 diabetes and then injecting these nuclei into unfertilized human eggs. Other researchers had tried this basic approach before. What the scientists at NYSCF and Columbia did differently was to leave the egg’s own nucleus intact.
To their surprise, this enabled the egg to be rebooted. That is, when the egg developed into a tiny embryo — smaller than a pinhead and containing fewer than 100 cells — the stem cells contained therein had nearly the same genetic profile as the diabetes patient. As a result, the researchers were able to successfully entice these stem cells to grow into other types of cells, including nerve cartilage and muscle tissue.
The scientists hope their approach could ultimately be used to develop insulin-producing cells that could help individuals with diabetes. The NYSCF and Columbia scientists haven’t attempted to do this yet, because the embryos they created were abnormal, having an extra set of chromosomes that originated from the egg. For this reason, they say, additional research is needed before their method is clinically useful.
“In this three-year study, we successfully reprogrammed skin cells to the pluripotent state,” says Dieter Egli, a senior scientist at NYSCF and an adjunct associate research scientist at CUMC. “Our hope is that we can eventually overcome the remaining hurdles and use patient-specific stem cells to treat and cure people.”
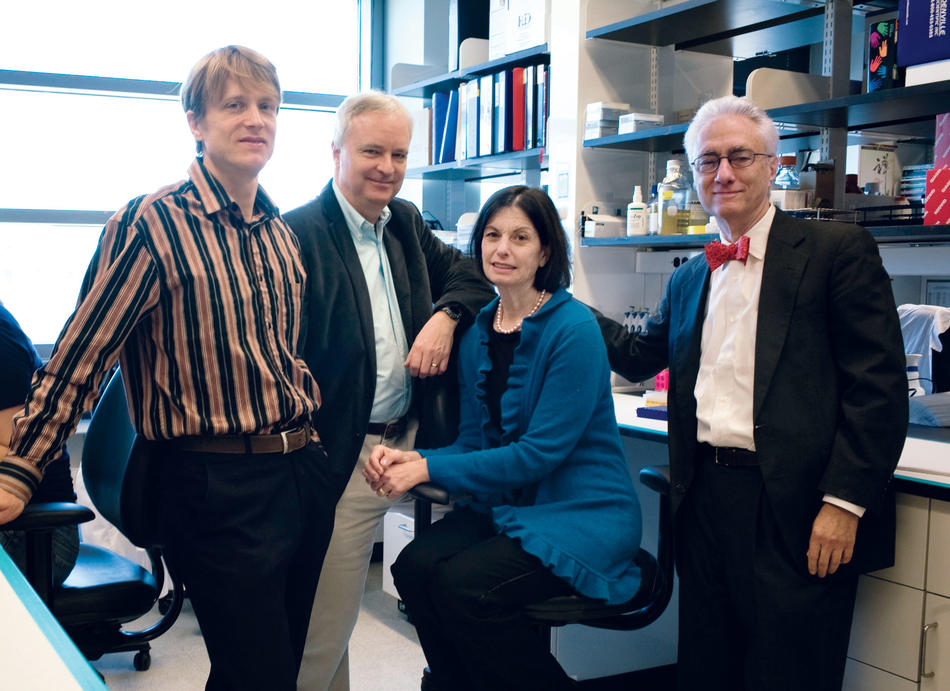
The lead authors of the paper were Egli and Scott Noggle, who is the principal investigator of NYSCF’s scientific team. Other Columbia scientists involved in the study were Mark Sauer, vice chairman of CUMC’s department of obstetrics and gynecology as well as its chief of reproductive endocrinology; and Robin Goland and Rudolph Leibel, codirectors of Columbia’s Naomi Berrie Diabetes Center.
“This is an important step toward generating stem cells for disease modeling and drug discovery,” says Leibel, “as well as for ultimately creating patient-specific cell-replacement therapies for people with diabetes or other degenerative diseases or injuries.”