Avery von Roeschlaub is a precocious seven-year-old. He solves geometry problems at a sixth-grade level, he’s obsessed with chess and all things outer space, and lately he’s been insisting that his dad, Kurt, a computer programmer, read to him at bedtime about black holes from a high-school astronomy textbook.
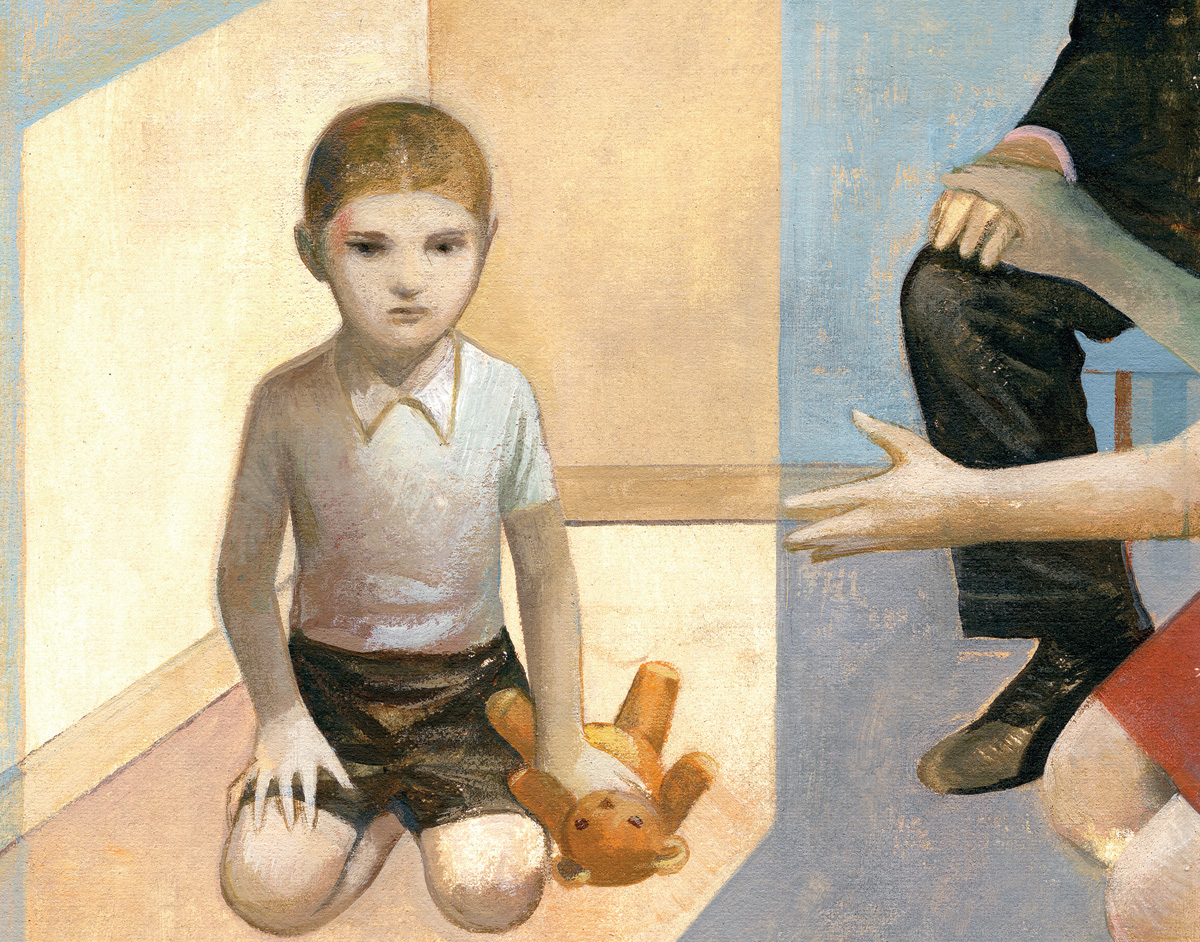
When it comes to reading people, though, Avery is out of his depth. “If somebody gets mad at him or tells a joke, he just doesn’t get it,” says his mother, Diana, an elementary-school teacher. “If another kid lies to him, he’s oblivious. He assumes everything you say is true. It makes him very vulnerable.”
Kurt and Diana, who live in Port Washington, New York, became concerned for their son when he was three. Avery’s vocabulary and speech were exceptional for his age, yet he couldn’t put words to his emotions. Unable to communicate if his legs got tired on a walk, Avery would become frustrated and burst into tantrums, writhing on the ground until he was physically restrained. He also seemed incapable of appreciating other people’s needs. “For me,” says Diana, “the aha moment came one afternoon when, after an incredibly exhausting day of tantrums, I told Avery to take a timeout and give me a rest. I remember him looking up at me and asking, ‘Why are you doing this to me, Mom, when I haven’t done anything wrong?’ That hit me like a ton of bricks. I thought, ‘Oh, my gosh, he really isn’t aware of what he’s doing.’”
Soon, the von Roeschlaubs decided to have Avery evaluated for autism. They were astonished to learn, however, that there are no direct tests. Whereas some mental disorders — such as the common forms of mental retardation, fragile X and Down syndromes — are detectable by the presence of particular genes, autism leaves no apparent fingerprint. All that doctors can do is observe a child and tally up his odd behaviors. If the child displays six distinct types of social and communication problems, then, according to the Diagnostic and Statistical Manual of Mental Disorders, he’s autistic. That means he’s eligible for costly behavioral therapy in public schools. But if he displays five or fewer symptoms, he’s likely to get labeled with attention-deficit hyperactivity disorder (ADHD), nonverbal learning disability, or any of several other, milder conditions that share many of autism’s symptoms.
“It’s hard to know when you’re dealing with autism versus some combination of other developmental problems, because there’s no one symptom or physical morphology that’s unique to the disorder,” says Bradley S. Peterson, the chief of child and adolescent psychiatry at Columbia University Medical Center (CUMC) and a leading autism researcher. “Autism is a bit of a mystery.”
That hasn’t stopped doctors from diagnosing it. The number of autism cases in the United States has doubled in the past decade, according to a report released by the U.S. Centers for Disease Control and Prevention (CDC) last December. About 1 in 100 eight-year-olds in the U.S. now has autism or a closely related “autism spectrum disorder,” which includes the milder Asperger’s syndrome and “pervasive development disorder,” a nonspecific diagnosis given to children with social and learning problems that don’t fit any other condition.
So what exactly is autism? Why are so many kids getting diagnosed with it lately? Scientists aren’t sure. They know that autism occurs when the brain’s memory and learning centers don’t develop properly, yet these same brain regions are abnormal in people with dyslexia, obsessive compulsive disorder, mental retardation, and ADHD. They know that physicians are increasingly aware of the condition and hence are spotting more cases, but they can’t rule out the possibility that something in our environment is triggering an epidemic. Some suspect that pollutants are contributing to the increase, but they can’t say which ones are most dangerous.
Columbia scientists are about to provide some answers. Peterson, for example, has begun identifying small sections of the brain that work differently in people with autism. W. Ian Lipkin and Mady Hornig, meanwhile, are determining which chemicals trigger the condition in children with particular genes. Later this year, these researchers will release findings that they say could help doctors identify youngsters who are susceptible to developing autism — and possibly take steps to prevent it.
Inner Work
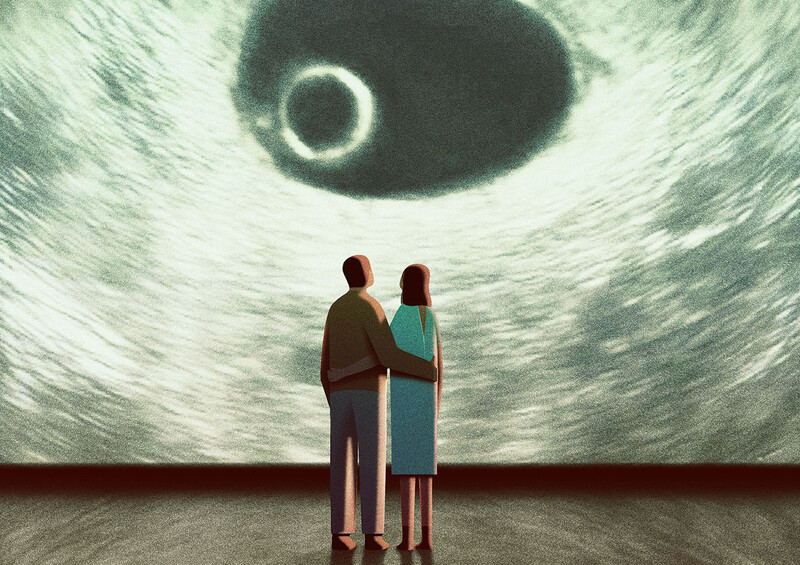
On a recent Tuesday morning, Avery was eased into the dark tunnel of a magnetic resonance imaging (MRI) scanner at Columbia. With both hands, he clutched his favorite stuffed puppy. Diana stood just outside the tunnel, caressing his leg. Once Avery was lying still, he was shown a movie in a pair of video goggles — human faces appeared, one at a time, wearing expressions that were demonstratively happy, angry, frightened, or sad. As Avery watched the faces, and as the MRI machine clanged and thwacked and moaned, a team of Columbia MRI technicians looked down at a monitor displaying an image of the boy’s brain.
“This region, here, is the one we’re interested in,” Peterson explained afterward, pointing to a thimble-sized section at the front of the brain called Broca’s area. “It’s involved mainly in language and higher-order social functioning.” This part of Avery’s brain was relatively still for most of the MRI session, but whenever Avery was shown a face, blood rushed into the area — indicating a spike in synaptic activity — and then, when the image of the face disappeared, the brain region got still again.
Over the past year, Peterson has examined the brains of more than 100 children and adults diagnosed with autism at Columbia’s Developmental Neuropsychiatry Program (DNP) clinic. He hopes to find distinguishing characteristics of autistic people’s brains to help doctors diagnose the disorder. A timely diagnosis is crucial, he says, because autism’s symptoms can be eased with therapies that encourage children to communicate their basic needs, perform simple tasks like getting dressed and going to the bathroom, and empathize with people. “The earlier you start the treatment,” Peterson says, “the better chance it has of making a difference. If we can help a child talk about his emotions, for instance, we might alleviate some of the tantrums.” Unfortunately, while autism’s symptoms are usually apparent by age three, he says, the disorder typically goes undiagnosed for several more years.
Avery’s first step as a research subject was to receive a free autism screening at the DNP, which is one of the nation’s top centers for autism care. The Columbia experts concluded that he has Asperger’s syndrome. “A lot of our clinical work here involves correcting diagnoses made by doctors who aren’t trained to make distinctions between autism and similar conditions,” says Peterson, who also treats patients. “We’ve seen autism misdiagnosed as everything from mental retardation to seizure disorders.”
In fact, Avery’s parents brought him here to participate in the research to shore up his diagnosis. “When Avery was three, doctors told us that he might have a developmental problem, but that it definitely wasn’t autism,” Diana says. “A year later we were told it could be Asperger’s. The process seemed kind of subjective.”
Until now, scientists have been unable to find any unique aspects of the autistic brain, according to Peterson, because MRI technology has limited researchers to assessing the size and shape of rather large brain sections. To address this challenge, Peterson has worked with Ravi Bansal, an associate professor of clinical neurobiology, to develop computer algorithms capable of quantifying blood flow and synaptic activity in millimeter-squaresized plots of brain tissue. In 2009, they were the first scientists to describe unique brain features that mark depression; they found that people with depression have 30 percent less brain tissue on the cortex, or surface, of their right hemisphere. And in a paper to be published later this year, Peterson and Bansal will argue that people with autism have less tissue in Broca’s area, as well as in nearby brain regions involved in language and social processes, than do people with other mental disorders.
“If you’d asked me five years ago when we would have a machine to spot autism, I would have said ‘Never,’” says Peterson, who is also the Suzanne Crosby Murphy Professor in Pediatric Neuropsychiatry. “Now, I think we could be using this technology in our clinic within a couple of years. If we could put a kid into an MRI scanner and determine that he has high-functioning autism versus, say, a combination of ADHD and a speech disorder, that could make a significant difference in the treatment plan we create.”
Further research is needed, Peterson says, to verify that the brain abnormalities he’s observed aren’t present in people who have other mental illnesses. But his preliminary findings are so strong that he and colleagues at the Developmental Neuropsychiatry Program are already discussing how MRI tests might be used to identify children as young as one or two who are at risk for developing autism. Peterson says that if behavioral therapies are administered to at-risk children this young, it’s possible that some cases of autism could be prevented altogether.
He arrived at this conclusion by using a clever study design: Peterson scanned the brains of healthy people who have an autistic sibling and discovered that they share the same malformed brain areas. “This means that the brain abnormality doesn’t determine you’ll have autism,” he says. “Rather, it gives you a susceptibility to it.” Other factors clearly are at play, and this gives Peterson hope that something might be done to prevent autism’s onset. “If we get a young kid in here who’s showing early signs of developmental problems and he has this brain abnormality,” he says, “we might consider beginning treatment before the diagnosis is even made.”
Unsimple Minds
In the past five years, scientists have identified some 10 genes associated with autism. You might think that by now doctors would be able to diagnose the condition with genetic tests. Autism is, after all, one of the most heritable illnesses. Scientists know this from studying identical twins — when one twin has autism, the other is much more likely than someone in the general population to have it. Yet, unlike some genetically based diseases, such as fragile X syndrome, whose causes can be traced back to a single gene, autism is suspected to involve as many as 100 genes that are as yet unidentified. That’s because autism is what’s called a “spectrum disorder,” not a neatly defined condition with a single physiological pathway, but a loose collection of symptoms that often occur together, for reasons that are unclear to scientists. These symptoms may all have their own genetic underpinnings.
To locate genes that cause illnesses, scientists usually work backward, from the physiological traits that characterize an illness to the chromosomes that build and maintain those parts of the body that are broken. And in this way, Peterson’s research could provide a map for finding more autism genes. If Peterson can demonstrate that a malformed Broca’s area contributes to the disorder, for instance, other scientists likely will examine any genes known to carry the blueprint for Broca’s area to see if they’re linked to autism.
Most autism experts, Peterson included, believe that genetic tests one day will be an important tool for assessing a person’s susceptibility to the condition. Scientists can already read an infant’s genome by analyzing blood taken from an umbilical cord. “The trick is that we have to figure out what physiological traits distinguish autism before we can find those genes,” Peterson says. “And we’re still a long way from understanding what’s going wrong in the neurological system of an autistic person.”
Today, one of the most ambitious efforts to describe the physiological basis of autism is taking place at Columbia’s Mailman School of Public Health, across the street from Peterson’s CUMC laboratory. There, W. Ian Lipkin and Mady Hornig are studying how environmental factors — everything from pollutants to viral infections to certain foods — can disrupt neurological development in ways that lead to autism. But if autism is hardwired into a person’s DNA, can chemicals really be that important? Lipkin says they play a pivotal role. “Genes go a long way in determining how susceptible a person is to autism,” he says, “but you may still need that final straw to trigger the illness.”
Unfortunately for public health efforts, it’s nearly impossible to determine the most dangerous risk factors for a population as a whole, says Lipkin, the John Snow Professor of Epidemiology and director of Mailman’s Center for Infection and Immunity. That’s because chemicals affect individuals differently. “Some scientists today say they’re going to find the environmental cause for autism,” he says. “That’s way too simplistic.” Lipkin suspects that certain at-risk children may develop autism from exposure to, say, ordinary levels of heavy metals, while others may become ill from using plastic containers; still other autistic children, he says, may become sick from an unlucky combination of factors, such as if a child is conceived by parents in their 40s, suffers from a prenatal infection, and then gets exposed to pollutants shortly after birth.
If only scientists could untangle how these genetic and environmental risk factors interact, then doctors might be able to prevent autism in individual children. Imagine if your pediatrician could tell you, based on your child’s unique genetic or metabolic profile, which pollutants to avoid.
Lipkin and Hornig believe this will be possible within a few years, at least for children with some of the better-understood vulnerabilities. And to sort through the swarm of variables, they’re now collaborating with the Norwegian government on an enormous public-health study that aims to discover the causes of many common illnesses, including autism, by tracking the health of some 110,000 people over their entire lives. Between 1999 and 2009, Norwegian scientists, as part of this wider effort, called the Norwegian Mother and Child Cohort or Mor og bärnundersokelsen (MoBa), recruited to their study pregnant women who allowed scientists to monitor the health of their children beginning in the womb. Scientists who participate in MoBa, such as Lipkin and Hornig, learn about their young subjects’ every illness, immunization, and medical treatment. They’ve also taken blood samples from the youngsters, who today range in age from one to nine, to see what pollutants, bacteria, and viruses they’ve been exposed to.
Lipkin and Hornig, who are medical doctors as well as research scientists, spent years working with the Norwegians to determine what clinical information MoBa would collect specifically to study autism. Because the MoBa data will be analyzed by scientists around the world, as well as by Lipkin and Hornig’s research team at Columbia, the Norwegians are gathering information that could be used to test dozens of hypotheses, some of them rather obscure, about autism’s causes. For example, MoBa scientists have asked mothers to document whenever they ate folate-enriched food while they were pregnant, because some scientists have argued that either elevated or reduced levels of this B vitamin may contribute to autism; they’ve asked parents to report their child’s every minor stomach complaint, because certain gastrointestinal problems have been linked to autism.
“If five years down the road, the research community has concluded that autoimmune dysfunction, or abnormal levels of vitamin B, or mercury exposure is a huge risk factor for autism, people will be scrambling to get their hands on our data, because it will show how all of these factors are operating,” says Hornig, an associate professor of epidemiology. “There’s really no comparison to what we’re doing here, in scale or in scope.”
Slicing up the Spectrum
One theory that’s received a lot of press in recent years is that measles, mumps, and rubella (MMR) vaccines lead to autism, but this idea is now widely dismissed by scientists. Lipkin and Hornig, in a landmark 2008 study, found no association between MMR vaccines and autism; parents may perceive a link, they say, because autistic children tend to show their first symptoms around the same age they get vaccinated.
According to the Columbia scientists, there’s better evidence to suggest that autism results from exposure to heavy metals like mercury and lead; phthalates found in some fragrances, shampoos, cosmetics, and nail polishes; phenols used in plastics; and polybrominated diphenyl ethers used as flame retardants in computer keyboards, building materials, and in other common products. Previous studies have also pointed to some pain relievers, anti-inflammatory drugs, and sedatives, as well as to men fathering children later in life. (Columbia epidemiologist Ezra Susser’s work has been instrumental in showing how paternal age is linked to autism.) However, most previous studies have been too small to eliminate the possibility that one risk factor was masquerading as another, say Lipkin and Hornig. They’re now gathering data, through MoBa, to assess all of these risk factors in a comprehensive way. “If you want to consider the relative dangers of these risks, and certainly if you want to know how they’re combining forces,” says Lipkin, “you need to conduct a very large population study.”
When Lipkin and Hornig began analyzing their MoBa data last year, they looked first at a chemical whose connection to autism had never been studied before: vitamin D. The idea that vitamin D deficiency contributes to autism has been floating around for a few years. There’s plenty of circumstantial evidence to suggest a connection: Rates of both vitamin D deficiency and autism are high among people with dark skin, which acts as an ever-present sunscreen. This is true especially among Africans who live in Europe and North America, where the need to dress warmly presumably limits their sun exposure. Also, there’s the fact that autism rates have been increasing during the same period that health officials have been telling us to avoid the sun, which is the source of 90 percent of our vitamin D.
The scientists’ hunch was a good one. When they looked for metabolic differences between the Norwegian children who’ve been diagnosed with autism versus those who don’t appear autistic, they discovered that the autistic kids are three times as likely to have elevated levels of a protein found in people who are vitamin D deficient; the body produces it in a desperate attempt to squeeze as much benefit as possible from the vitamin D that it does receive. If Lipkin and Hornig can find further evidence that a shortage of vitamin D contributes to autism, they’ll look for genetic markers that could identify a child who is susceptible to vitamin D deficiency. They’ll also consider if additional risk factors can combine with vitamin D deficiency to make a child autistic. Hornig’s previous research provides some clues about what to look for. She’s demonstrated in laboratory studies that mice who experience viral or bacterial infections early in life go on to display autistic-like behaviors: They avoid each other and do back flips obsessively. Hornig suspects that a lack of vitamin D can exacerbate the dangerous effects of an infection, as the vitamin is known to bolster the immune system.
“If this turns out to be true, the clinical implications would be clear,” says Hornig, who hasn’t yet published the findings on vitamin D. “If your baby has a severe infection, this could tell doctors to watch his vitamin D levels, and maybe even give him vitamin supplements as a precaution.”
Only a portion of the autistic children in the MoBa study appear to be vitamin D deficient. But Lipkin and Hornig say that this type of targeted approach to autism research will lead to the best prevention methods and treatments. “There’s no one type of autism, just as there’s no one type of cancer,” says Lipkin. “And as we learn how different types of autism work, we’ll figure out ways to help subgroups of these children, one by one.”
For parents like Diana and Kurt von Roeschlaub, whose desire to understand their son’s suffering hasn’t ended with his diagnosis, that’s encouraging news. “When you find out your child has autism, you go through denial, anger, depression, and finally acceptance, which means accepting the child you have, rather than wishing he was the child you’d always imagined having,” Diana says. “But what never goes away is the desire for an explanation, both for yourself and so that you can validate your experience, and your child’s experience, to other people. You want it all to make sense, somehow.”