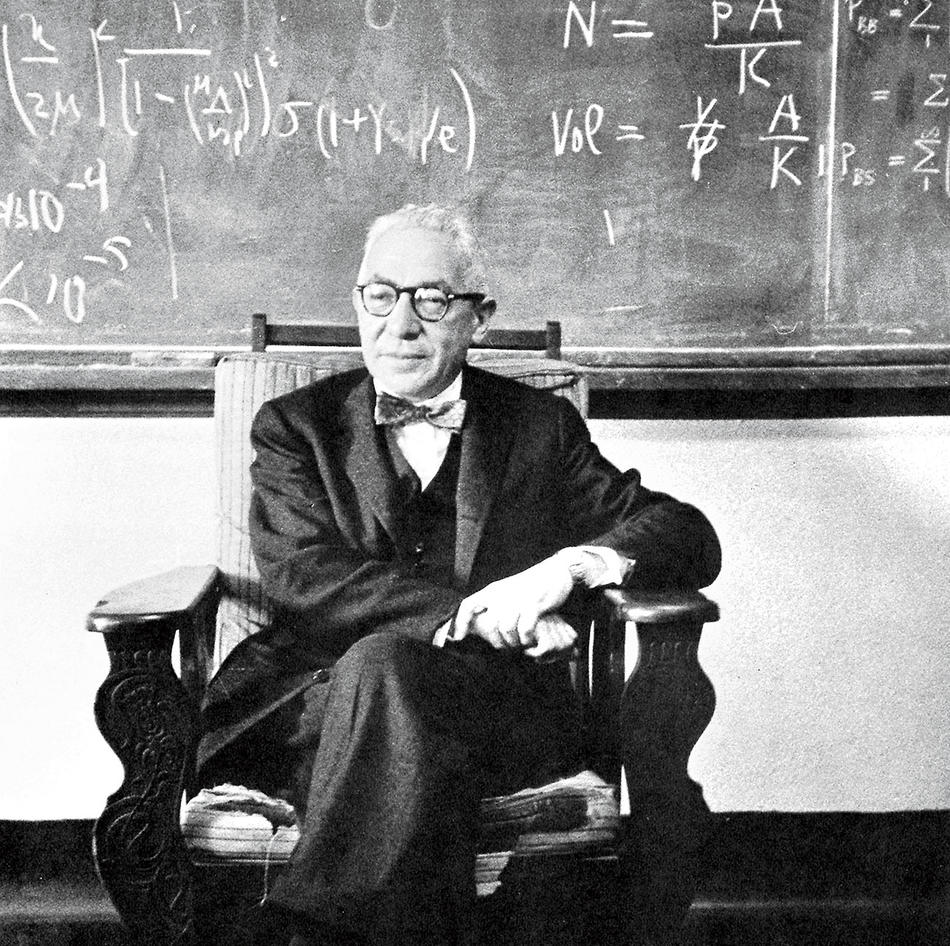
Rank your personal pantheon of famous scientists — Copernicus, Curie, Faraday, Fermi, Pauling, Pasteur — and Isidor Isaac Rabi ’27GSAS, ’68HON likely wouldn’t make the top tier. He is amply recognized, however, at Columbia’s physics and astronomy building on the Morningside Heights campus. There, in room 809 of Pupin Hall, his office of fifty years has been converted into the Rabi Room, a study lounge that also serves as a shrine to the man. A plaque honoring him is on the wall. So are more than twenty pictures of Rabi, along with his Nobel Prize medal in physics, awarded in 1944. Two students in the lounge, buried in work, readily acknowledge they’ve never heard of him. “I haven’t even looked at the photographs,” says one. Then the other, checking out the pictures, pauses to take in the accompanying text reciting Rabi’s accomplishments. “Wow, that’s crazy,” she says. “I should have known that.”
Born in what is now Rymanów, Poland, and raised in New York City, Rabi got his PhD at Columbia in 1927. Three years later, Columbia hired him for $3,000 a year. His lectures in theoretical physics were singularly awful, his students said — but his research skills were stunning. “I think physicists are the Peter Pans of the human race,” he told the New Yorker in 1975. “They never grow up, and they keep their curiosity.” That trait was encouraged by his mother, decades earlier; upon his return from school, she would say: “Izzy, did you ask a good question today?”
Rabi never stopped asking them, and after arriving at Columbia, he certainly answered some. Like any physicist of his generation, he was determined to unravel the conundrums of the atom; particularly intriguing were the protons, particles within the atom’s nucleus. Put simply, Rabi learned that protons — if placed in a magnetic field and hit by radio waves — generate an energy signal.
The medical application of that finding was not readily apparent to Rabi. No one imagined this signal might eventually be used to image the insides of the human body and detect heart disease or cancer. But the discovery of NMR — nuclear magnetic resonance — led to the development of MRI, magnetic-resonance imaging. Rabi’s insight, undeniably genius, ultimately ignited a multi-billion-dollar technology that may someday save your life. Perhaps it already has.
In the basement of the Jerome L. Greene Science Center on the Manhattanville campus is Tommy Vaughan’s “broom closet,” a room with little more than a desk, three chairs, and a whiteboard. Though not officially Vaughan’s office, the space is his “place to hide,” he says, “commandeered to get some work done.” As Director of Magnetic Resonance Research at the Mortimer B. Zuckerman Mind Brain Behavior Institute, he has much to do. The seventy-two studies he supervises at the school’s new Magnetic Resonance (MR) Research Center — his brainchild — “are only a beginning,” he says.
Vaughan is one of the world’s foremost MRI engineers. For thirty-five years, he has designed, built, and retooled MRI systems and applications; he holds more than fifty patents. Manufacturers in biotech and medicine regularly license his inventions. Yet he too seems to be just beginning. Recruited in 2016 from the University of Minnesota, he is preparing to radically accelerate MRI research at Columbia. “We are on the threshold of revolutionizing how we approach science and medicine,” he says.
Over the threshold, actually. Staffed primarily by Columbia neurologists and engineers, the MR Research Center is spread over four locations boasting eight MRI machines: three at Manhattanville’s Zuckerman Institute, three more at Columbia University Irving Medical Center, one at the New York State Psychiatric Institute, and one at the Nathan S. Kline Institute for Psychiatric Research in Orangeburg, about twenty miles north of New York City. Within the next year or so, another MRI will arrive at the Fu Foundation School of Engineering and Applied Science. Eventually, the center will have eighteen MRIs. No research institution in the world currently has as many. Rather than diagnosing patients, the MRIs will look for clues that may lead to cures for disorders and diseases of the brain: anorexia, alcoholism, Alzheimer’s, Parkinson’s, Huntington’s, schizophrenia, suicide, stroke — the list goes on, as do Vaughan’s plans.
“We can build a smaller, cheaper magnet that we can put anywhere,” he says. “Even in the middle of Inner Mongolia. Anywhere on the planet.”
After Rabi’s breakthrough, chemistry labs used NMR to examine organic molecules. “It’s how we know what sugars and proteins and DNA look like,” says Vaughan. By the time doctors began scanning patients in the early eighties, the name was an issue; public-relations-wise, NMR had an image problem. Patients couldn’t get past the N, as in nuclear. Some were convinced the scanner was dousing them with deadly radiation. NMR became MRI, the same concept yet sounding so much more benign. (More recently, some researchers have begun using the term MR.)
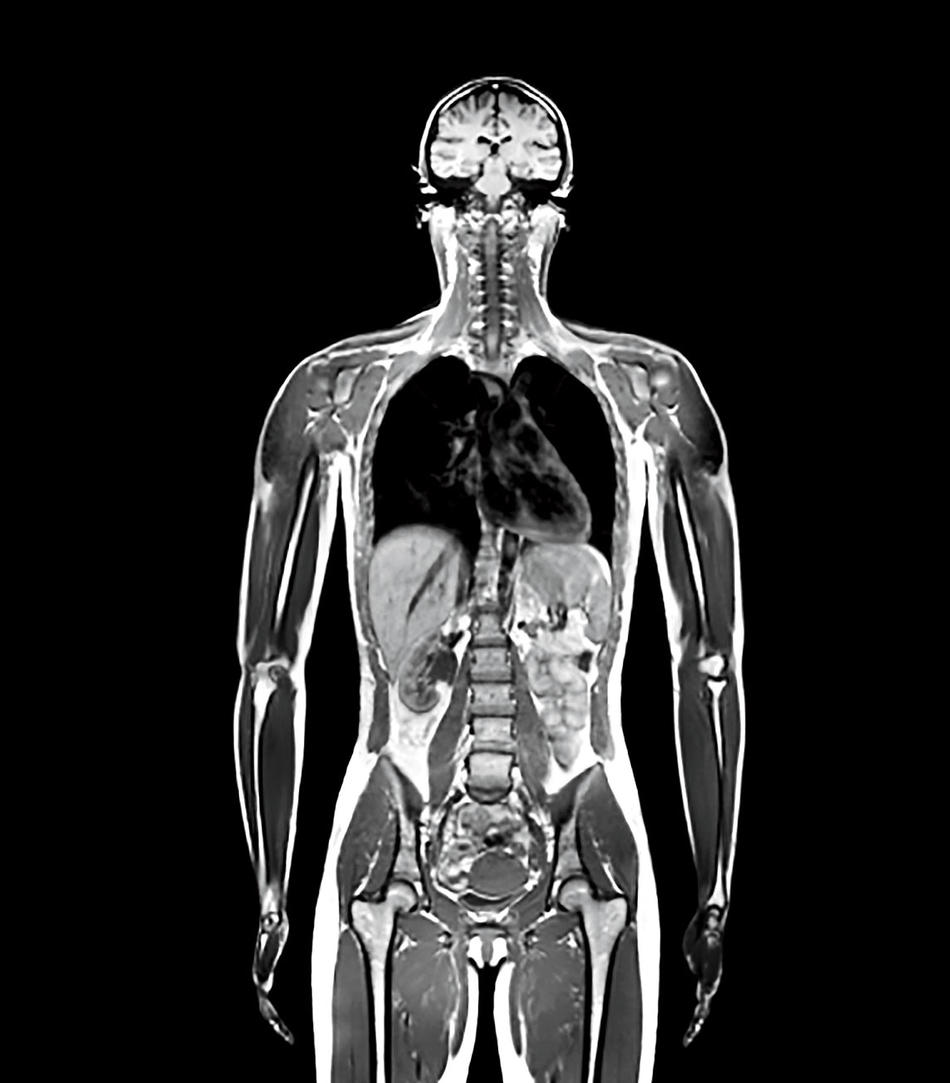
MRIs are no longer considered exotic. They have been imaging your organs, tissues, and bones for nearly forty years. They can see skin, muscle, blood vessels, tendons, tumors, joints, and ligaments in astonishing detail. Notwithstanding their scary trappings — the fifteen-ton magnet, those loud bangs, that oppressive and cramped space, the intimidating warnings posted everyplace — MRIs are painless and harmless.
“Magnetic-resonance imaging is completely radiation-free,” says Kathleen Durkin of the Zuckerman Institute. “You can get an MRI every single day of your life and be perfectly safe.” Conversely, X-ray machines do emit small doses of radiation and can’t image everything. They work best on hard tissue, like teeth and bones. “I hate this cliché,” says Vaughan, “but MRI is a one-stop shop for diagnostics, and also for science — for trying to understand how the body and mind work. This is the ultimate tool to noninvasively observe a living system.”
Of the millions of patients scanned, few know how the machine works. Yet for all their spookiness and sophistication, MRIs rely completely on the most common chemical compound on Earth — water. An MRI is all about water. And human beings “are walking bags of water,” says Durkin. Indeed, 60 percent of you is water. “And that water inside your body,” she says, “gives off a signal to the MRI.”
Every molecule of water is two atoms of hydrogen linked to one atom of oxygen. But only the protons in the hydrogen atoms send the signal. Walk into the MRI room and enter the machine’s magnetic field and trillions of hydrogen protons in your body snap to attention. “You don’t feel it,” says Durkin. But the procedure has essentially begun. Like iron filings near a toy magnet, the hydrogen protons align with the magnetic field.
Once on the MRI bed, the patient is pushed into the cylinder, which houses the magnet. In the MRI scanner is an antenna. It transmits radio waves. Invisible and innocuous, the radio waves ping your hydrogen protons. They absorb the radio waves. They spin in a different direction. Momentarily discombobulated, they need time to right themselves.
“As they realign,” says Durkin, “they spit back a signal, a little bit of energy.” That signal is a faint ricochet of the radio wave that hit them. A second antenna — a receiver, hidden in a coil near your head — intercepts the signal. Much the way your television set works, the MRI’s processing units unscramble the signal and reduce the noise, all straightaway. “And we get a brain picture out of it,” says Durkin. “Or a picture of an abdomen, or an ankle, or anything on the body.” From little more than subatomic blips, an MRI can discern a cancerous tumor.
It is difficult to fathom the power of an MRI machine. Wear or hold anything metallic or electronic within its magnetic field — major mistake — and you will find out. Your phone could fly out of your hand and smash into the machine. Pacemakers can become erratic. Large objects with metallic parts, like chairs, have been picked up and yanked into the cylinder.
It is also difficult to grasp how sensitive the machines are. For the MRI to work, the magnet must be supercooled to −452 degrees Fahrenheit, the edge of absolute zero. Any warmer than that and the magnet quenches. “That means it’s no longer superconducting,” says Vaughan. The damage to the machine can be considerable, if not irreversible. Liquid helium, the coolant, is scarce and expensive, and the MRI, with its dozens of kilometers of coiled wire, just chugs it.
Housing MRIs is a challenge. They take up lots of space — along with the machine, there’s the adjoining equipment and console rooms. “And the magnet has to be shielded from interference,” says Vaughan, which is why the walls of the MRI suites at the Zuckerman Institute are lined with thin sheets of copper. They block incoming radio waves; otherwise, signals from local radio and television stations would mingle with the MRI and distort the image.
The strength of an MRI magnet is measured in units of T, or teslas, in honor of the scientist Nikola Tesla. Says Durkin: “Have you ever seen one of those big magnets in the junkyard that picks up a car and brings it to get squished into a cube? That’s 1-tesla.” Two of the MRIs at the Zuckerman Institute (named “June” and “Eve”) are 3-tesla, triple that strength.
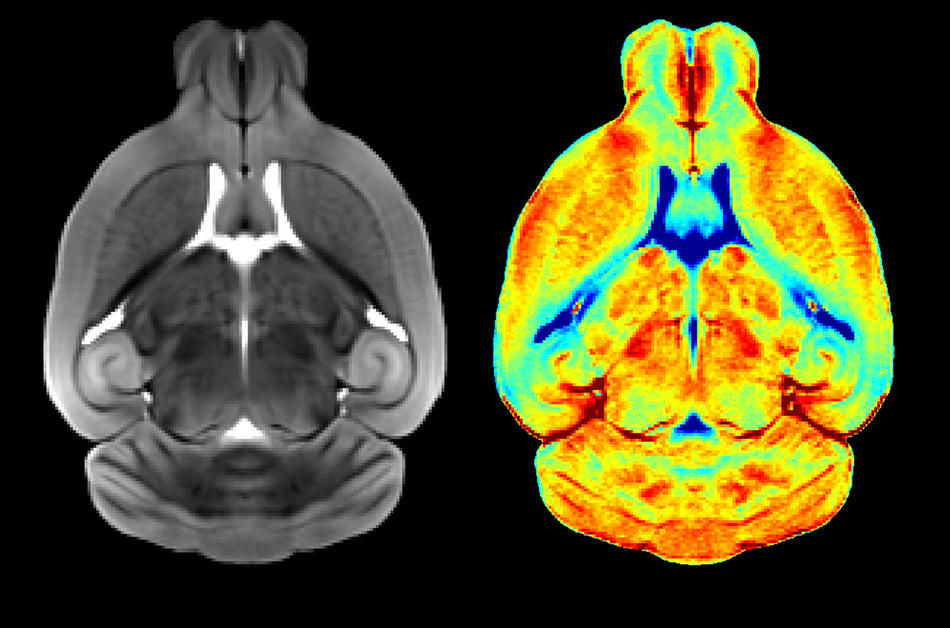
The stronger the MRI magnet, the higher the resolution, the greater the detail, the more useful the image; most hospitals do fine with a 1.5-tesla. Zuckerman’s third MRI, a 9.4-tesla (unnamed) is more than six times that, but with a trade-off. The stronger the magnet, the smaller the bore — the space where the subject lies down. “With a 9.4,” says Durkin, “the bore is so small that people can’t get in it.” Instead, the tiny tray is only large enough to hold mice. Within the next year or two, however, a 7-tesla will arrive at Zuckerman. People can fit in this one. Says Durkin: “The images are spectacular.”
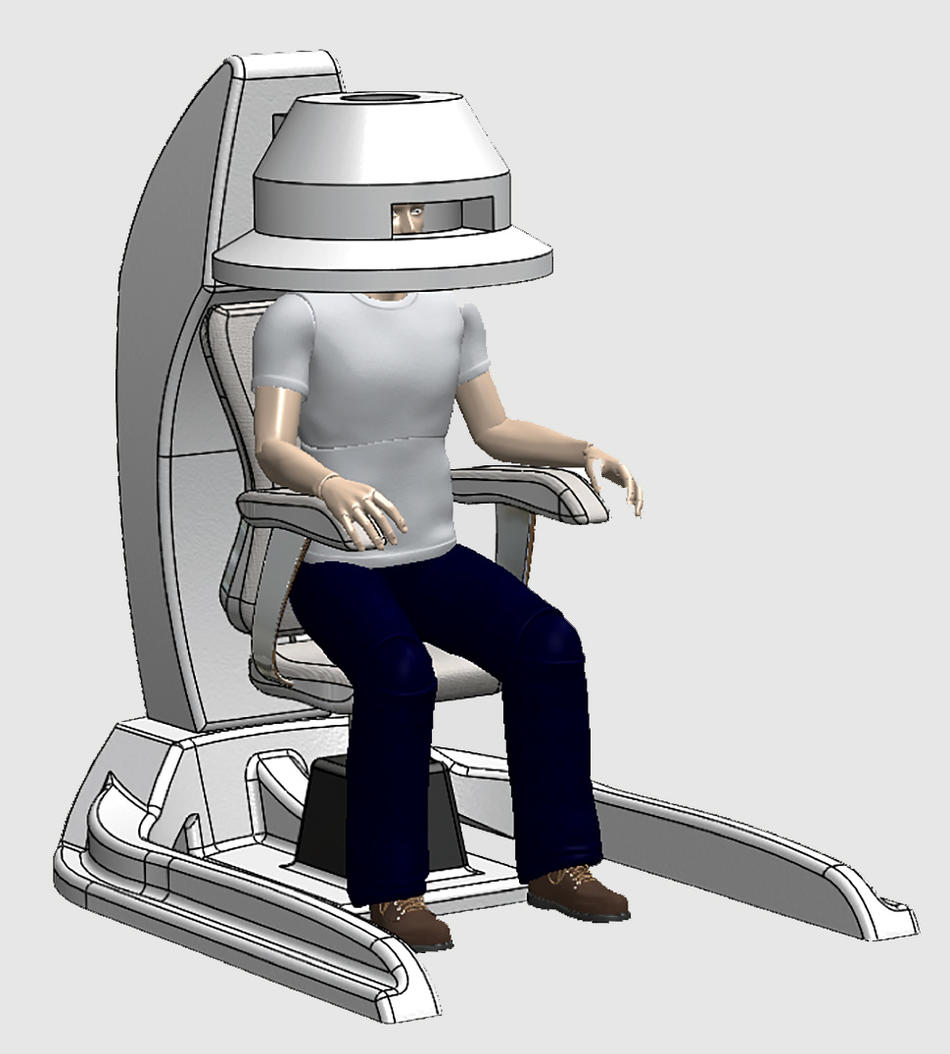
Right now, Vaughan is developing a 1.5-tesla MRI that’s a “head-only imager,” he says. “It looks like the hair dryer your mother sat under in the beauty parlor.” It should be ready in three years. Rather than record the brain activity of someone lying motionless inside a tube, Vaughn’s head-only MRI lets subjects sit in a chair with arms and hands free. Scientists will capture how the brain interacts with the body while someone weaves a basket, lifts weights, draws a picture, or plays the piano.
Columbia officially chartered the MR Research Center in 2018, and many of the studies are just starting. Although manufacturers like Siemens, GE, and Toshiba sell MRIs off-the-shelf (the cost is roughly $1 million per tesla), some machines require a reconfiguration of their hardware to accommodate the research. The modifications can take months. Some of the adaptations have never been done before.
One example: Ray Lee, a senior research scientist at the Zuckerman Institute, wants to see how brains respond as people touch, talk, and smile. So he designed “the world’s first dual-head MRI coil,” a way to put two subjects under one magnet and scan their brains simultaneously. “This is fundamentally different from all previous methodologies,” he says. “It’s a new way to study people interacting with each other.”
The old way demanded that researchers display photographs of a subject’s family and friends on a screen inside the bore and ask the subject to react to them. Real interactions —caressing a partner’s face, holding hands, and sharing quiet conversations — are obviously precluded. Lee expects “dramatic differences” with his invention. “When two people look at each other, there’s a real emotional exchange,” he says. “There’s much more brain activity than someone just looking at a picture.”
Yuval Neria, a professor of medical psychology at CUIMC, is trying to find out why some brains rekindle long-ago traumas rather than extinguishing them. Earlier research shows that symptoms of posttraumatic stress disorder — including anxiety, agitation, depression, flashbacks, and nightmares — may fade after a horrific event, only to reappear decades later, when the victim is in late middle age or older. “Aging is a big promoter of late-onset PTSD,” says Neria. “It can be very disabling.” Usually the trigger is “a new stressor,” like the loss of a spouse or a health problem. Such relapses are not uncommon in war veterans. For two or three decades after combat, many do fine; then a sudden loss changes everything.
The MRI can see those changes in three brain regions: the hippocampus, where memory is stored; the prefrontal cortex, where decisions are made; and the amygdala, the alarm center. If connections between them are muddled and the amygdala is malfunctioning, the brain “can’t discriminate between what’s dangerous and what’s safe,” Neria says. Everyday events can trigger flashbacks.
But solutions exist. With a grant from the National Institute of Mental Health, Neria compared MRI scans of patients before and after ten weeks of talk therapy. Telling the traumatic story again and again seems to help. The prefrontal cortex “dampens” the overly active amygdala, he says: “The brain is better connected. It has greater capacity to deal with the trauma.”
Without the MRI, Neria would have to rely on self-reporting, which is not always definitive. “We know after decades of self-reports how biased they are,” he says. “But with the MRI, you have data.”
Almost anyone who spends several hours at a rock concert or football game may notice afterward an annoying auditory artifact — ringing or roaring inside the ear. It could be high-pitched, like crickets screeching, or a dull rumble, like a jet engine during flight. Wait a few minutes or get a good night’s sleep and the blare usually goes away. But for some, the sound doesn’t stop. There will never again be a moment’s vacation from the noise.
The diagnosis is tinnitus. Medical experts rarely agree on anything about it, even the pronunciation (some say tin-NIGH-tus; others, TIN-uh-tus), but millions have it, and there is no cure. Cognitive-behavioral therapy can help, but for some the sound is so strident, they are virtually incapacitated. A few are so devastated they commit suicide. Half of US soldiers exposed to IEDs develop tinnitus, and 1.5 million veterans receive disability benefits for it, at a cost of $2 billion per year.
Diana Martinez, a professor of psychiatry at CUIMC, got tinnitus seven years ago after a flight from Hawaii to Newark. “It was a high-pitched buzz,” she recalls. “I felt like I was in the subway station all day long.” Martinez was lucky. Tinnitus, a mysterious disorder, occasionally disappears, and within a week, hers did. “Thank goodness,” she says. “It’s miserable.”
Martinez never forgot that terrible week. Her new $1.6 million study, funded by the US Department of Defense, will monitor forty volunteers. Previous research suggests that the brains of tinnitus patients have low levels of GABA, an amino acid believed to block anxiety (“a brake on the brain,” says Martinez). Injections of ketamine, a common anesthetic, could help; earlier findings show ketamine boosts GABA in the prefrontal cortex. Increase GABA in the auditory cortex, the part of the brain that processes hearing, and tinnitus may diminish.
With the MRI, it’s easier to tell if the ketamine is working. As with Neria’s PTSD study, Martinez can ask patients if they’re feeling better, but survey responses are subjective. With patients in the scanner, the MRI can image the change in GABA levels after the ketamine injections. “It’s the best way to look,” says Martinez. A half billion people worldwide may benefit from her research.
Doing the research is one thing. Delivering the data to the world is another. Vaughan has thought of that too.
“Since day one,” he says, “we have saved all of our MR data in the cloud.”
This is a first, at least for MRI research. Laboratories, limited by storage capacity, once had to toss old data to make room for more. But for the past year and a half, the Zuckerman Institute has stockpiled its gobs of data in the cloud on a customized Google platform. Eventually, advanced machine learning will scrutinize the data in a fraction of the time it would take a researcher. “This will be the future,” says Vaughan. “It just has to be.”
And it will be another beginning: Vaughan hopes Columbia will be the prototype for a worldwide network of cloud-based data. Consortiums of researchers could connect. Looking for clues to cure autism, PTSD, tinnitus, and a thousand other disorders? Just access the cloud and analyze the data from millions with the same problem. “If the data set is big enough,” says Vaughan, “you can ask a question, get a correlation, and answer any medical question you could imagine. The cloud is like your mind. The more information you have, the smarter you are. This opens up a whole new world.”
But today, 90 percent of the world has no access to MRIs. “The machines are big, heavy, fragile, and expensive,” Vaughan says. Throughout much of Asia, Africa, and South America, they are not affordable, deliverable, or maintainable. “We need a completely different kind of magnet,” he says. “One we could bring to the developing world. One that can go on the back of a truck and bounce on a bumpy dirt road to a village in Guatemala.”
For that to happen, the magnet and scanner need to be one-fifth the size and weight of current models, yet furnish just as good an image. Vaughan is working on it. With a miniaturized unit, cost is less. Delivery is easier. Solar battery systems or a generator could supply power. That standard three-room suite becomes a single room. For the coolant, the costly liquid helium could be replaced with nitrogen, an inert gas that composes nearly 80 percent of Earth’s atmosphere. “It can be liquefied right out of the air,” Vaughan says. And a clinic’s MR system, no matter how remote, could send data by satellite link directly to the cloud. “You could run a worldwide lab from your desk,” he says.
“Imagine having access to billions of patients, collecting and storing data from everybody,” says Vaughan. “At that scale, you could study every disease or behavior or characteristic known to man.”
A group of international investors — based in China, Malaysia, Korea, Taiwan, and the United States — has asked Vaughan to develop a more accessible MR system. That pilot program, if it flies, might expand throughout the world. In the US, a next-generation MRI might one day sit in the corner of a doctor’s office in Manhattan. Walk-in clinics will be in shopping malls. That data would go to the cloud too.
How long before all this happens? “A decade,” he says. “In a decade, everyone will see this in place, and spreading fast everywhere.” Even in Mongolia? “Yes,” says Vaughan. “Even Mongolia.”
This article appears in the Fall 2019 print edition of Columbia Magazine with the title "The Mind Readers."