On a Thursday evening in early October, as the Ebola outbreak in West Africa was starting to make international headlines, nearly two hundred students and professors gathered in an auditorium at Columbia’s engineering school to learn how they could help. Earlier in the day, Mary C. Boyce, dean of Columbia Engineering, and Linda P. Fried, dean of the Mailman School of Public Health, had sent an e-mail to all members of their schools, inviting anyone interested in developing “low-cost, technology-driven” solutions to the crisis to come out and learn more. Those who received the e-mail were encouraged to spread the word to anyone else at the University who might want to help.
“We weren’t sure if anybody would come,” says Boyce. “It was during midterm exams, after all. But we wanted to move fast.”
The organizers ended up getting an enormous response, with students and faculty from across the entire University turning out. The Columbia Design Challenge was on.
The meeting began with W. Ian Lipkin, an epidemiologist at the Mailman School of Public Health, describing a few ideas he had for inventions that might help field workers in West Africa do their jobs more safely and effectively. Lipkin, who is one of the world’s leading microbe hunters, had firsthand experience working in such situations, having been on the ground in Asia during the SARS epidemic and in Saudi Arabia during the outbreak of the respiratory virus MERS; he knew many people now risking their lives in the fight against Ebola. Over the previous few weeks, he told the audience, he had heard from his colleagues that much of the equipment they were using was ill-matched to the conditions. The polyethylene-coated suits they wore to protect themselves from infected bodily fluids, for example, became excruciatingly hot in the tropical sun, forcing them to disrobe and cool off every forty-five minutes or so. They were consequently changing out of several contaminated suits each day, increasing their risk of touching infected fluid. Their method of disinfecting the suits — spraying one another with bleach before disrobing — was also problematic, since they could easily miss spots.
“Maybe you could build some sort of cubicle they could step into and get sprayed down more thoroughly,” said Lipkin. “They’d have to be able to breathe the whole time, of course. I don’t know if that’s feasible. You’re the engineers.”
Another challenge facing the field workers was how to disinfect their cell phones and handheld diagnostic tools. The current strategy was to put them in ziplock bags, pour in chemical powders and water to produce chlorine gas, and then run away before the bags burst open.
“You need to get out of there so you don’t inhale the toxic gas,” Lipkin said. “This is insane.”
He imagined a solution: a sturdier container, perhaps made of thick plastic, into which electronic devices could be placed for safe disinfection. “This would be extremely helpful,” he said. “Health-care workers are dying because they don’t have good decontamination procedures.”
Rachel Moresky, another Mailman faculty member in close contact with people working in West Africa, brought the conversation back to the hazmat suits. The suits were problematic not just because they couldn’t be worn for long periods of time, she said, but also because they hampered health-care workers’ ability to perform even simple tasks while wearing them.
“Imagine trying to insert an IV into a patient’s arm when you’re wearing this space suit with three pairs of gloves in 120-degree heat and your goggles are fogging up with sweat,” she said.
Lipkin piped up again: “Maybe we could devise some way to keep them cool inside the suit. That would be huge.”
The attendees, after listening to descriptions of these and other logistical challenges, were told they had twenty-four hours to come up with solutions. Anyone wishing to participate in the design challenge, sponsored jointly by the engineering and public-health schools, was invited to pitch ideas to a panel of professors and safety experts the next afternoon. Those who brought the most promising ideas would receive small seed grants to create prototypes, which would need to be ready for testing within a month. Along the way, Lipkin and others would solicit feedback on the inventions from colleagues in West Africa.
Lipkin’s parting instruction: keep it simple. Think twice, he said, before trying to develop new diagnostic tools, therapeutic drugs, or other complex technologies that major companies were already working on. Focus instead on quick-and-dirty inventions that companies were unlikely to develop for a lack of potential profit.
“Think to yourself,” he said, “what can I achieve in a short time frame, on a very small budget, that will save lives?”
Quick thinking
At 1 p.m. the next day, eighteen teams showed up with ideas. One group of undergraduates, led by engineering junior Jason Kang and College juniors Katherine Jin and Kevin Tyan, said they had come up with a better way to decontaminate hazmat suits. They proposed adding a blue dye to the bleach that field workers were using. Spraying a garment would temporarily turn it blue, thus helping workers determine when every square inch of a suit had been cleaned.
“The trick will be figuring out the right combination of chemicals so that the pigment isn’t broken down by the bleach right away,” said Kang, who is studying to be a biomedical engineer.
Ponisseril Somasundaran, a professor of mineral engineering, came with a different way to decontaminate hazmat suits: he suggested that a sprayable bleach foam would work better than a liquid spray, since it would more effectively cling to the suits’ waterproof surface. The foam, he said, would also be ideal for decontaminating entire hospital rooms, ambulances, and airplanes, because less bleach would be required in relation to the liquid spray to do the same job.
“The bleach runoff from a liquid spray is not an insignificant environmental issue,” Lipkin said later. “This makes good sense.”
Seven more teams, most of them led by students, received the panel’s support, along with preliminary grants of $150 each to begin working on prototypes. Among their ideas was to create an “inverse” personal-protection suit that Ebola patients would wear while being transported and which would comfortably contain and absorb their bodily fluids so as not to infect others; a folding wooden cot with a plastic underbelly to catch bodily fluids during sickness; a cooling vest that health-care workers could wear beneath a hazmat suit; and a text message-based communication system that would alert health-care workers to the latest outbreaks.
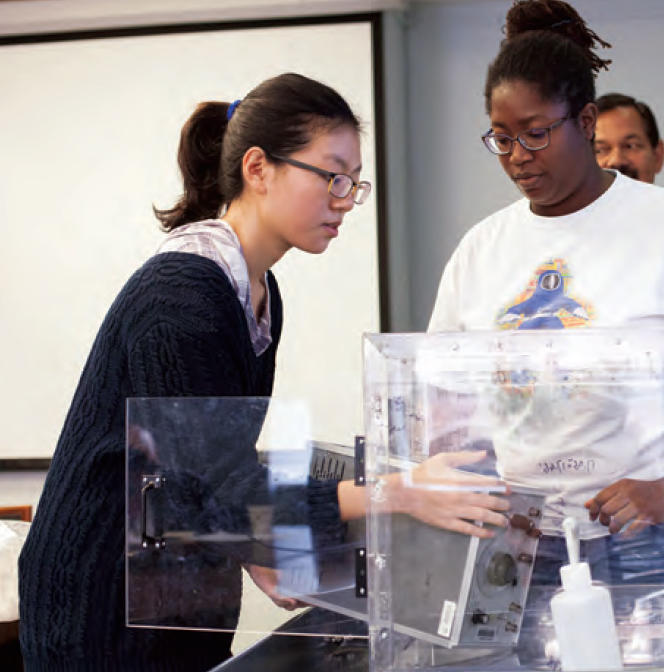
Some teams hewed closely to the suggestions Lipkin had made the previous day. A group led by Jun Guo and Kay Igwe, both engineering students, took up the challenge of creating a fumigation chamber for electronics devices. They proposed building an eighteen-inch acrylic cube with a drawer for putting in chemical powders and a valve for adding water; objects as large as desktop computers could be placed inside. Its walls would be translucent so that sunlight would break down the resulting chlorine gas, thus allowing the chamber to be opened safely within minutes.
“It looks like a good preliminary design — just make sure the resulting gas pressure doesn’t cause the chamber to explode,” said Jeffrey Kysar, the chair of Columbia’s mechanical engineering department, who, along with Lipkin, Boyce, biomedical engineering professor Aaron Kyle, and several other faculty and staff members, sat on the review panel.
Other teams went in unexpected directions. One group proposed making aprons with West African-inspired prints that could go over hazmat suits to make health-care workers look less intimidating. The project was inspired by media reports about some West Africans being reluctant to visit treatment centers in part because their staffers looked so frightening. “This is an anthropological approach to the issue,” said Daniel Taeyoung ’09CC, ’13GSAPP an adjunct assistant professor at the School of Architecture, Preservation, and Planning. “We want to help alleviate the reticence or hostility that some people might feel when encountering the workers.”
In a "maker space"
Over the next few weeks, the sixty or so design-challenge participants worked long hours, somehow balancing their jobs and class schedules with the drive to create new sprays, foams, suits, apps, and cots. Much of the work was done at the engineering school’s “maker space,” a facility that combines elements of the machine shop, wood shop, and design studio.
The team led by Guo and Igwe used the maker space to build their fumigation chamber — first designing it with AutoCAD software and then manufacturing a prototype with a laser cutter. “We solicited help from lots of friends in working out the design,” says Eric Tong, a key member of their team. “A classmate who is studying materials engineering was instrumental.”
Jin, Kang, and Tyan, in order to make their colorful bleach-spray additive, spent many late nights teaching themselves about chemical dyes and disinfectants. They soon decided that adding a surfactant, which is a chemical that helps liquid adhere to surfaces, would make a bleach spray even more effective on waterproof hazmat suits. The team spent $650 on various dyes, surfactants, and other additives in search of the right combination.
Along the way, the judges offered guidance. They reminded the students to consider how the West African heat would affect chemical reactions, for instance.
By early November, the new concoction was ready for testing. In a preliminary trial conducted in a biosafety level 3 laboratory at Columbia University Medical Center, a team of professional hazardous-material experts sprayed it on garments covered in West Nile and influenza viruses.
“The beautiful thing about bleach is that it kills all viruses and bacteria,” says Lipkin. “So as long as the bleach could still be sprayed with these new additives in it, it would kill Ebola — or anything else. And it worked fine.”
New tools for emergency workers
The first invention likely to be deployed in West Africa is the fumigation chamber. In December, its creators received $2,000 from the engineering and public-health schools to produce five units. The team, which has grown to include engineering undergraduates Jumari Robinson and Ajit Singh, is now working to finish the chambers; Lipkin plans to send them to colleagues at the National Institutes of Health and the Centers for Disease Control and Prevention who are overseeing Ebola-response efforts in both West Africa and the United States.
“It’s an extremely simple invention that we’ve tested and demonstrated is safe,” he says. “It’s a no-brainer that people in the field will want to use it.”
At least three more inventions from the Columbia Design Challenge appear to have a good chance of being widely deployed. One is the blue bleach spray. The New York City Fire Department recently purchased two hundred units of it from Jin, Kang, and Tyan.
The chief medical officer of the department, David Prezant ’77CC, contacted the students after reading a New Yorker article that described their project. The FDNY performed its own tests using their mixture of additives in December and subsequently decided that its hazardous-materials emergency teams could use it in responding to any of a variety of viral or bacterial outbreaks.
“Disinfecting hazmat suits has always been a challenge for us,” said Prezant. “Imagine it’s a windy night in New York and you’re working in the dark. In conditions like that, it’s especially tough to know if you’ve sprayed the suit well. The solution that these kids came up with is phenomenal.”
Also likely to make a real-world impact, Lipkin says, are the foam bleach spray created by Somasundaran and an ingenious hazmat suit with internal cooling pouches and a camel-style hydration pack for sipping water through a straw — the work of engineering undergraduates Ritish Patnaik, William Smith, Joshua Bazile, and Sidney James Perkins. Both of these inventions were finalists in a national design contest organized by the US Agency for International Development this winter. While neither Columbia team won that competition, the resulting media exposure piqued the interest of potential collaborators. DuPont, one of the world’s largest manufacturers of hazmat suits, for instance, recently contacted Patnaik and his classmates about incorporating some of their innovations into the company’s products.
“We think our suit could be worn comfortably for up to three hours,” says Patnaik, who is studying to be a biomedical engineer. “And in the hands of the right manufacturer, each could be produced for a few dollars.”
As far as dean Mary Boyce is concerned, the success of these projects demonstrates not only the social consciousness of Columbia students and faculty, but also their entrepreneurial and collaborative spirit.
“From the beginning, I looked at this primarily as an educational project, one in which young engineers would learn how to work with public-health experts and others to deliver real-world tools in a rapid-fire atmosphere,” says Boyce. “We hoped that some of their designs would be useful in the field. But I don’t think any of us could have predicted the level of success that we’ve actually seen.”