Scientists and clinicians from across the University pivoted this year to address the worst pandemic in a century. Here are just a few ways they are working to develop new treatments, diagnostics, and prevention methods.
AIDS researchers design lab-grown antibodies to both treat and prevent coronavirus infection.
Today, as dozens of scientific groups around the world race to create vaccines for COVID-19, some researchers are quietly pursuing a complementary strategy: developing medicines called monoclonal antibodies. Experts say these drugs, which are laboratory-grown, genetically supercharged versions of immune cells that the body produces to fight the novel coronavirus, could have a dual benefit, providing an effective treatment to those who already have the disease while giving healthy people immunity against COVID-19 for up to six months. This temporary immunity would help serve as an emergency stopgap until vaccines become widely available.
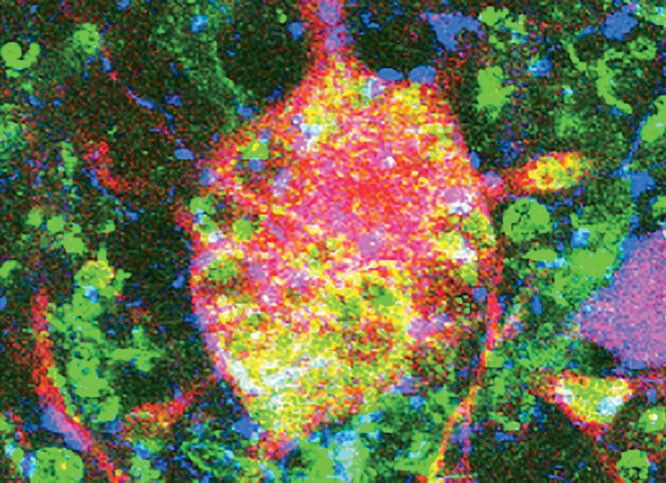
At the forefront of the effort to develop monoclonal antibodies is a group of scientists led by David D. Ho ’00HON, the director of Columbia’s Aaron Diamond AIDS Research Center and the Clyde and Helen Wu Professor of Medicine. Since last spring, when Ho reorganized his twenty-five-member team to focus on COVID-19, he and his colleagues have been working around the clock on the project, analyzing blood plasma donated by COVID-19 patients at Columbia University Irving Medical Center to identify naturally occurring antibodies that might be useful in developing therapies. (The term “monoclonal” denotes that the antibodies are mass-produced from the same parent cell and are therefore identical.)
“A patient will typically generate hundreds of antibodies against a particular virus, and what we’ve been doing is assessing which are the most effective at binding to the novel coronavirus and therefore preventing it from invading healthy cells,” says Ho, whose team has previously developed monoclonal antibodies used to treat HIV/AIDS. “We then genetically tweak them to make them even more potent.”
Ho says the antibodies, if manufactured as drugs and administered to COVID-19 patients at the first sign of infection, could dramatically reduce the severity of the illness. “The body can take up to two weeks to generate its own antibodies against a virus, so we’d be bolstering its defenses in that initial two-week period,” he says.
Given to healthy people, Ho says, monoclonal antibodies could prevent infection altogether, as the antibodies would swarm and mark for destruction any COVID-19 viral particles the instant they appeared in the body, before they took root and began to replicate. In this way, monoclonal antibodies would act like a vaccine, but with a key difference: whereas a vaccine provides long-term immunity by teaching the body to recognize and respond to an invader on its own, monoclonal antibodies are merely hired hands whose protective effects will fade as they gradually wear out and disappear from the bloodstream.
A key benefit of monoclonal antibodies, though, is that they are easier and faster to develop than vaccines. And for this reason, proponents of the drugs believe that monoclonal antibodies for COVID-19 are likely to be made available before vaccines are approved and distributed to everybody who needs them.
The Columbia scientists recently took a big step toward achieving that goal, describing in the journal Nature the chemical structures of dozens of powerful COVID-19 antibodies that they have used to successfully prevent the disease in hamsters. These antibodies, the scientists say, are among the most potent coronavirus-fighting immune cells yet identified, and also among the most diverse, with some targeting the novel coronavirus in previously unobserved ways. Ho and his colleagues are now planning further studies in people and collaborating with pharmaceutical companies to turn the antibodies into drugs.
In addition to having widespread applicability as a treatment, Ho says, the drugs would provide a desperately needed prophylactic for the elderly, people with underlying health issues, and health-care workers.
“And it’s likely that the antibodies will be useful even after vaccines are available, because vaccines often don’t work well for the elderly,” Ho says.
The Columbia scientists are also hoping to develop antibody drugs that could be made cheaply available in the developing world. “We believe that we may be able to make certain monoclonal antibodies effective at unusually low doses, which could make them more affordable and enable nonprofits to distribute them widely in poor countries, where people are usually the last ones to receive new medicines,” Ho says.
Data reveal fatal consequences of delayed response.
One the world’s leading groups at forecasting the spread of infectious diseases, led by Jeffrey Shaman ’03GSAS at the Mailman School of Public Health, has been looking back at COVID-19 case numbers to assess the impact of public-policy decisions made in response to the pandemic.
In one recent paper, the researchers showed that if social-distancing measures had been imposed just one week earlier in the United States — beginning March 8 instead of March 15 — at least seven hundred thousand COVID-19 cases and thirty-six thousand deaths nationwide would have been avoided. “A small amount of time can make a big, big difference,” says Shaman, whose analysis is based on computer modeling. “Catching an outbreak in its initial growth phase is incredibly important in reducing the numbers of deaths.”
Newer, safer UV lamps could spell lights out for coronavirus.
As restaurants, shops, and other small businesses look for ways to curtail the spread of COVID-19, a promising new prevention strategy — the use of continuous low doses of ultraviolet (UV) light to kill microbes — has emerged from Columbia’s Center for Radiological Research.
“This is a safe solution that can eradicate airborne viruses minutes after they’ve been breathed, coughed, or sneezed into the air,” says David J. Brenner, a professor of radiation biophysics and director of the center.
Scientists have long known that UV light has the capacity to destroy viruses, bacteria, and other microbes. In fact, germicidal UV lamps have been used for decades to sterilize surgical theaters, research labs, ventilation ducts, and food-processing plants. During the pandemic, New York City has used the technology to clean its subway trains, blasting the interiors of the cars with UV beams. But to do this they must shut the transit system down, since conventional germicidal UV lamps can damage the skin and eyes and can only be used in unoccupied areas.
Now Brenner and his colleagues say they have improved the existing technology by developing a UV lighting system that can kill microbes without penetrating human cells — thus making it suitable for use in crowded public spaces. (Their system uses far-UVC light, which is further down the UV spectrum and has shorter wavelengths.) “If you’re indoors with lots of other people, you really want that environment to be continually sterilized,” he says.
After nearly eight years of research and multiple long-term studies, Brenner says his team has confirmed the technique’s safety and demonstrated that it can wipe out a wide variety of pathogens, including the viruses that cause influenza and measles, drug-resistant bacteria, and several coronaviruses that are responsible for common colds. The researchers are now testing the technology on SARS-CoV-2 — the coronavirus that causes COVID-19 — in collaboration with Mailman School virologists W. Ian Lipkin and Thomas Briese.
“Our results so far are very encouraging,” says Brenner, noting that far-UVC light appears to be just as effective against SARS-CoV-2 as it is against other microbes. He also suggests that far-UVC lamps could be retrofitted into existing light fixtures to help control future pandemics as well as COVID-19.
Several companies, including the Florida-based Healthe and Japan’s Ushio, have already begun manufacturing germicidal lamps based on the Columbia team’s technology, in anticipation of the ongoing experiments with SARS-CoV-2 proving successful.
“Far-UVC light could be used in combination with other preventive measures, like wearing face masks and social distancing, to limit the transmission of SARS-CoV-2 and other viruses in hospitals, nursing homes, buses, planes, trains, schools, restaurants, offices, theaters, gyms, and anywhere else that people gather indoors,” Brenner says. “It could greatly reduce the level of airborne virus in these environments.”
Fertility researchers create faster, cheaper test.
Scientists at the Columbia University Fertility Center have repurposed an RNA test that they had previously developed to spot genetic abnormalities in embryos to detect coronavirus in saliva samples. The researchers say their new COVID-19 test is faster, cheaper, and easier to use than existing diagnostics and could improve access to testing throughout the country.
“Our test will generate results in about thirty minutes, whereas others can take several days,” says Zev Williams, director of the center and chief of reproductive endocrinology at Columbia University Irving Medical Center. “And it doesn’t require an uncomfortable swab up your nose — all you do is spit in a cup.”
The Columbia team’s key innovation, Williams says, has been to streamline the process by which genetic samples are analyzed. Usually COVID-19 tests require samples to be run through expensive equipment that is only available in large laboratories — thereby requiring most health clinics to send out their samples for analysis. The Columbia test, he says, enables medical workers to process the samples and interpret the results onsite. They simply place a patient’s saliva in a plastic tube filled with reactive enzymes and then submerge the tube in warm water. If the tube turns yellow, the test result is positive; if it turns red, it is negative.
“To combat this virus, we need to test widely and frequently and get the results back quickly,” says Williams. “This requires a paradigm shift in how we go about testing for it.”
In late July, the biopharmaceutical company Sorrento Therapeutics announced its intention to bring the new Columbia test to market; the company’s scientists are now working with Williams’s team to validate its accuracy. They hope to soon pursue “rapid, full-scale production” in the US.
“Once we obtain regulatory approval, we envision the test being used to screen people before they board an airplane, visit a nursing home, or go to school or summer camp,” Williams says. “The test could also be a more affordable option for health-care facilities in developing countries where outbreaks have overwhelmed their testing and logistical capabilities.”
Study reveals the mysteries of a complex and shape-shifting disease.
From the start of the pandemic, doctors and nurses have been confounded by the coronavirus’s ability to migrate outside the respiratory tract and invade other parts of the body, including the heart, liver, kidneys, stomach, skin, and nervous system.
Now, in an effort to help other medical workers anticipate COVID-19’s mercurial moves and treat it more effectively, a team of Columbia physicians has published the first comprehensive review of the disease’s physiological effects, describing how and when it may attack different organ systems. The study, which appears in the journal Nature Medicine, was spearheaded by Aakriti Gupta ’19PH, a Columbia cardiology fellow who was among a large number of doctors temporarily deployed to Columbia University Irving Medical Center’s special COVID-19 intensive care unit when the pandemic hit New York City in early March.
“I was on the front lines right from the beginning, and I observed that patients were clotting a lot, they had high blood sugar even if they didn’t have diabetes, and many were experiencing injury to their hearts and kidneys,” Gupta says. “It seemed like every day my colleagues and I were observing some new symptoms.”
Over the next few weeks, Gupta and Donald Landry ’83PS, the chair of medicine at Columbia’s Vagelos College of Physicians and Surgeons, brought together nearly thirty physicians from Columbia, Harvard, Yale, and several other institutions to collect and review information about the multiple manifestations of COVID-19. Their study, which draws on reports from hundreds of medical teams around the world as well as their own clinical observations, provides a detailed portrait of a stunningly complex disease.
According to the paper, the coronavirus’s shape-shifting nature is explained in part by its compatibility with a protein receptor — a kind of molecular portal into cells — called ACE2, which is present in most organs. Possessing the biological equivalent of a master key, the coronavirus can enter, genetically commandeer, and ultimately destroy cells throughout the body; its invasion of the kidneys, for example, is likely responsible for high rates of renal failure among COVID-19 patients, while its incursion into the circulatory system contributes to the formation of blood clots that cause heart attacks, strokes, and myriad other problems.
But the virus’s direct assault on the body is only part of the story. The researchers say that some of the disease’s worst effects appear to be caused by an overzealous immune response. That is, the body’s natural defense system, in its determination to purge infected organs of diseased cells, may flood the organs with too many white blood cells, which are the body’s foot soldiers against microbial invaders. This can end up inadvertently damaging healthy tissue.
Knowing all the ways that the disease is likely to attack and determining the best treatments in each case requires an extraordinary amount of scientific and clinical knowledge, the Columbia researchers say.
“This virus is unusual, and it’s hard not to be impressed by how many manifestations it has,” says Mahesh Madhavan ’14PS, a CUIMC cardiology fellow who contributed to the paper. “We hope that our review, observations, and recommendations can help other clinicians in places where cases are now surging.
New insights on animal vectors.
Three times now this century — with SARS, MERS, and COVID-19 — a bat coronavirus has jumped into humans and caused a pandemic. How concerned should we be about this happening again?
Simon Anthony, a Columbia epidemiologist, recently mapped the evolutionary histories of SARS-CoV-1 and SARS-CoV-2 — the coronaviruses behind SARS and COVID-19 — to learn how and when they acquired the ability to infect humans and to understand the environmental factors that may give rise to such instances of “zoonotic spillover.” He found evidence that SARS-CoV-2 is part of a long lineage of bat coronaviruses that have for decades possessed the ability to infect humans and have periodically imparted this power to other coronaviruses, including an ancestor of SARS-CoV-1, by swapping DNA with them. Such instances of genetic recombination between viruses frequently occur in the bellies of bats, which are infamous for harboring large numbers of pathogens.
Anthony says that his team’s research underscores the need for better surveillance of viruses in wildlife, especially in Southeast Asia and east-central Africa, where coronaviruses of the lineage that includes SARS-CoV-2 are known to circulate. “We need more detailed information about these coronaviruses and the hosts and locations in which they’re found,” he says. “This will help us evaluate the risk they pose to humans.”
Columbia doc flips protocol and finds a solution to a critical-care crisis.
In her two decades as a critical-care doctor, Sanja Jelic had never confronted a situation as serious as the one that unfolded at Columbia University Irving Medical Center on April 6, at the height of the coronavirus pandemic in New York City. On that day, eight patients under her care went into acute respiratory distress at once. Struggling to breathe even with the help of oxygen masks, all of them needed to be intubated and hooked up to ventilators. The problem was that CUIMC’s staff could only intubate a few people at a time, which created a bottleneck.
“I had never seen so much strain on our ICU resources,” says Jelic, an associate professor of medicine. “We had to do something to buy time.”
So Jelic improvised, asking a few of her patients to roll onto their stomachs and lie face-down. This clinical maneuver, called proning, is often used with pulmonary patients who have already been connected to ventilators and sedated, since it has been shown to help an unconscious person’s lungs absorb oxygen. Physicians had rarely attempted it with conscious patients, though, deeming it of little benefit. And yet Jelic and her staff, within an hour of helping several patients turn onto their bellies, were shocked to find that they improved so dramatically that they no longer needed ventilators at all.
“It was a wonderful outcome, not only because we conserved resources but because we spared these patients from being intubated, which is not without its risks,” Jelic says.
Jelic’s discovery — which she and colleagues subsequently replicated in a small study of eighty-eight patients published in the journal JAMA Internal Medicine — has since inspired caregivers across the country to experiment with the practice. In many states now experiencing spikes in COVID-19 cases, proning has emerged as a cheap and easy way for health workers to help critically ill patients.
“It’s not always an adequate replacement for ventilation,” Jelic says. “But as a stopgap measure where resources are stretched thin, it is worth trying and can certainly help.”
And while larger clinical trials are still needed to determine the specific circumstances in which proning may or may not benefit COVID-19 patients, Jelic says she has no doubt that her team’s unorthodox methods improved care, and possibly saved lives, at CUIMC.
“When you’re practicing medicine in extreme conditions, sometimes you need to think creatively to give your patients a fighting chance,” she says. “If you’re inundated with critically ill people, you can’t throw up your hands. You have to find another way.”
Global project to address medical workers’ mental-health issues.
Working long hours under constant threat of infection, medical workers around the globe are facing tremendous risks, not only to their physical well-being but to their mental health. In the wake of COVID-19, many report feeling burnout, anxiety, and depression.
To ensure that they get the support services they need, researchers at Columbia’s Mailman School of Public Health, together with colleagues in Chile, have launched a major study of the pandemic’s mental-health impacts on medical workers in more than thirty countries. Over the next year, the researchers, led by Ezra Susser ’74CC, ’82PS, ’93PH, a Columbia professor of epidemiology and psychiatry; Franco Mascayano, an epidemiology doctoral student; and Rubén Alvarado, a psychiatrist at the University of Chile, will track the mental health of thousands of doctors, nurses, and medical support staff in Argentina, Chile, Germany, Ghana, Guatemala, Italy, Japan, Nigeria, Saudi Arabia, Tunisia, Turkey, and other nations.
“We want to understand who is most vulnerable,” says Susser, who is also conducting a similar study on health-care workers in New York City. “This research will yield data of immediate utility to health systems and governments on questions such as how to prioritize mental-health treatment and other support services.”