Earlier this year, the American Psychiatric Association conducted its annual poll on anxiety. Americans, the survey found, are more worried than ever. They’re worried about the economy, politics, gun violence, runaway technology, and climate change, on top of the usual angst over relationships and health. They’re also more depressed: according to the Centers for Disease Control and Prevention, major depressive disorder, also called clinical depression, afflicts sixteen million people a year and is a leading contributor to other illnesses and to disability, absenteeism, and substance abuse. Anxiety and depression often overlap, and in the past twenty years prescriptions for antidepressants have risen nearly 50 percent.
“It’s a massive problem,” says David Hellerstein, a research psychiatrist at the New York State Psychiatric Institute and a professor of clinical psychiatry at CUIMC. “Yet in the last several decades, there’s been a significant underinvestment in solutions.”
Hellerstein is one of a growing number of clinicians who are investigating a potential answer: the little understood, highly promising, very illegal class of drugs known as psychedelics. These substances, which include psilocybin (a hallucinogenic compound found in more than two hundred species of mushrooms) and LSD (derived from the ergot fungus, which infects grains such as rye), deeply alter perception and mood, and new clinical trials suggest that they may help a host of psychological conditions, including depression and generalized anxiety disorder — with only minor side effects and virtually no risk of addiction.
As expectations grow for the medical acceptance of these drugs, Columbians are helping to shape the psychedelic-therapy future. They are conducting clinical trials and studies, synthesizing new compounds, training students in psychedelic-assisted therapy, and insisting that the emergent industry be guided by ethics, sound science, equity, and respect for the wisdom and welfare of Indigenous communities that have used psychotropic plants for millennia.
Hellerstein became interested in the medical possibilities of psychedelics in the 1990s and is now a site principal investigator on the largest analysis of a psychedelic drug in history: an international multisite study of psilocybin for treatment-resistant depression, sponsored by the biotech company Compass Pathways. Because the US government lists psychedelics as Schedule I drugs — meaning they have “no currently accepted medical use and a high potential for abuse,” according to the US Drug Enforcement Administration — clinical trials are difficult to arrange. Thus the government and mainstream pharmaceutical companies have largely refrained from funding psychedelic research, leaving a few small biotech startups to raise money and navigate the regulatory maze. “You have to jump through a lot of hoops to get licensing to secure sourcing and storage of the drugs,” Hellerstein says.
To be eligible for FDA approval, a drug must pass three phases of investigation, with increasingly large numbers of subjects, to establish its efficacy, side effects, and safety. In 2022, the New England Journal of Medicine published the results from phase two of the Compass Pathways study, which compared the effects of different doses of synthetic psilocybin on 233 people and found that the largest dose was the most therapeutic. “A day after treatment, there was a profound change in depression symptoms in the patients treated with the high dose of twenty-five milligrams,” Hellerstein says. “That’s really different from the SSRIs, such as Lexapro or Zoloft, which have a very gradual onset.”
SSRIs (selective serotonin reuptake inhibitors) are the most commonly prescribed medications for depression and anxiety. These drugs prevent neurons in the brain from reabsorbing serotonin, a neurotransmitter that regulates mood. It can take weeks or months before patients start to feel better. “With psychedelics, most studies have found improvement in just one or two treatments,” says Hellerstein. “And the effects can last for months. These are very rapidly acting drugs that have a major disruptive effect on brain activity.”
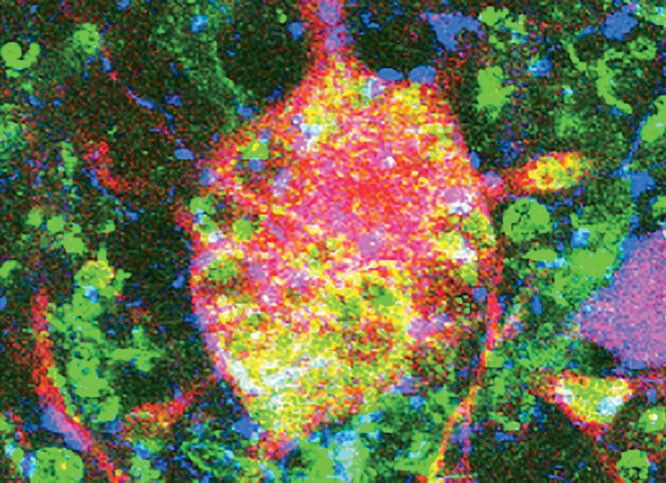
As Hellerstein explains, in people with depression there is often overactivity in parts of the brain that involve negative self-talk, so that they get stuck in a rut of despair, repeating bad thoughts like a broken record. “Psychedelics seem to scramble those neuronal connections and help people to skip over the grooves and move into new ways of thinking,” he says. “There’s more growth of connections between brain cells, whereas depression and other psychiatric disorders are characterized by fewer connections from one nerve cell to another.”
Whereas SSRIs work by gradually altering serotonin activity in the brain, psychedelics stimulate a subtype of serotonin receptors, the 5-HT2A receptor (a receptor is a protein on the membrane of a brain cell), triggering a chain of chemical events inside the neuron. “These drugs have a different mechanism of action than existing antidepressants,” says Hellerstein. “They seem to induce communication between different brain networks that do not normally talk to each other, so that the network connections that we have in normal life — you see a tree and think ‘tree,’ or you hear a horn and see a car and put it together in your brain to construct meaning — are scrambled. Instead, you may see sounds or hear colors or have other distortions of perception and thinking. This scrambling of connections causes these very profound, intense experiences during the trip. After the trip has faded, the patterns of brain connection can persist for days and weeks, and in some yet-to-be-understood way seem to have a positive effect on mood and other psychiatric symptoms.”
The Compass Pathways study for treatment-resistant depression is now in phase three. But close on its heels in the race for FDA approval is the nonprofit drug manufacturer Usona Institute, which is in phase-three testing of psilocybin for major depressive disorder. Natalie Gukasyan, an assistant professor of psychiatry at CUIMC, was a co-investigator on the Usona study. She points out that what makes the psychedelics studies different from others, and so tricky to negotiate with the FDA, is that they include a psychotherapy component — an anomaly for an agency designed to assess food and drugs.
The trials typically work this way: after a lengthy screening process, people with depression participate in a several-hour preparatory session. Therapists talk with each participant about their case history and explain what to expect from the drug. Participants are then seated in a quiet, comfortable room and swallow a pill of synthetic psilocybin (or a placebo). They can put on eyeshades for darkness and headphones for music. The therapists then mostly “sit back and let the person have their experience,” Gukasyan says. “They monitor the person’s blood pressure and tend not to interfere with what’s going on. They’re just there to support them. It’s not unusual for the person to start talking or to seek some reassurance or comfort.”
After the treatment, participants attend a series of follow-up “integration” sessions in which they process the thoughts and feelings they had experienced while medicated. Gukasyan notes that what occurs in the integration visits depends partly on the style of the therapist. “We need some better research on what works in therapy,” she says.
Like the Compass Pathway trials, the Usona study has been promising: on average, participants who took the drug became less depressed than they had been and less depressed than those who got the placebo, and Gukasyan has led further research showing that these positive effects can last for up to a year. “The caveat there is that a lot of things can happen over the course of the year to keep those scores low,” says Gukasyan. “Some subjects go off to get their own therapy or go back into conventional treatment. But there’s at least some evidence that for a subset of people, the effects can be quite durable.”
Psilocybin isn’t the only hallucinogen in the spotlight. While depression gets the mushroom treatment, generalized anxiety disorder is being put, you might say, to the acid test.
Daniel Karlin ’01CC, ’05GSAS, chief medical officer for the pharmaceutical startup MindMed, recently led a twelve-week phase-two clinical trial for generalized anxiety disorder, a condition affecting 6.8 million Americans and marked by obsessive and debilitating worry over small, everyday matters. The drug under investigation is arguably the most controversial of all psychedelics: lysergic acid diethylamide, or LSD. The MindMed study is the first trial for LSD in the US in more than fifty years.
First synthesized in a lab in the late 1930s, LSD, known to recreational users as “acid,” was a burning topic of psychiatric inquiry through the 1950s and early 1960s. But as it seeped into the general population and became synonymous with countercultural excess and paranoid freak-outs, the media began touting its dangers, real and invented. The US outlawed LSD in 1968, and in 1970 President Richard Nixon signed the Controlled Substances Act, which banned all psychedelics and ended further medical research. So strong was the backlash against LSD, with its anti-establishment and psychotic associations, that when researchers began re-exploring psychedelics in the 1990s, starting with mescaline and psilocybin, LSD was still considered too hot to handle.
“People have this internal experience where they see themselves through a different lens.”
No longer. Karlin and his team of researchers tested the efficacy of LSD at four different doses and saw remarkable results. “The day after dosing, folks had significantly improved anxiety symptoms versus placebo,” Karlin says. “In the one-hundred microgram group we saw about 50 percent go into remission from their generalized anxiety disorder. And that remission persisted out to week twelve. So people went into remission earlier and generally stayed in remission through the end of the study.”
Unlike the psilocybin studies, the MindMed LSD trials, while closely monitored for safety, do not include psychotherapy. “In essence, there’s sort of an autotherapeutic process that occurs, so we didn’t do therapy,” Karlin says. “The process is more inward: people have this internal experience where they see themselves through a different lens.”
The buzz around these studies reflects a dramatic shift in attitudes about psychedelics, one driven by disparate voices, from military veterans suffering from treatment-resistant depression and PTSD (earlier this year, the VA announced it would fund new research into psychedelics) to writers like Michael Pollan ’81GSAS, author of How to Change Your Mind: What the New Science of Psychedelics Teaches Us About Consciousness, Dying, Addiction, Depression, and Transcendence. In that book, which was published in 2018 and adapted into a Netflix series, Pollan consumes LSD and psilocybin, and his account of ego loss while under the influence may elucidate the high success rate of the clinical trials.
“When the ego dissolves,” writes Pollan, “so does a bounded conception not only of our self but of our self-interest. What emerges in its place is invariably a broader, more openhearted and altruistic — that is, more spiritual — idea of what matters in life.”
The term “psychedelic” was minted in 1957 by British psychiatrist Humphry Osmond, one of a small number of doctors who performed experiments with the drugs (he used LSD to treat alcohol addiction), which were new to Western medicine. LSD was first synthesized in 1938 by Albert Hofmann, a Swiss chemist who was trying to develop a drug to stimulate the circulatory and respiratory systems. In 1943, Hofmann accidentally ingested the substance and had such an incredible adventure that he began dosing himself intentionally and chronicling the effects (“Kaleidoscopic, fantastic images surged in on me, alternating, variegated, opening and then closing themselves in circles and spirals, exploding in colored fountains ”).
Word of this magical drug spread to psychiatrists around the world, who took it themselves and cataloged their own response: feelings of connection to nature, intense perceptions of beauty, detached introspection, openness, loss of fears and anxieties, and spiritual elation. They believed that these extraordinary effects could be harnessed for use in psychotherapy.
One of these intrepid psychiatrists was Sidney Cohen, who studied pharmacology at Columbia and conducted many LSD experiments in the 1950s. Cohen first tried LSD in 1955, advocated for psychiatric trials, and published several books on the drug. Historian Benjamin Breen, a former Columbia postdoc and the author of Tripping on Utopia: Margaret Mead, the Cold War, and the Troubled Birth of Psychedelic Science, calls Cohen “one of the most consequential people in the history of psychedelic therapy.”
“Cohen was pretty open about using LSD and benefiting from it himself,” says Breen. “This was really important — the whole idea of a participant observer. He was trying to find a middle path where these substances would be legal but could be safely used with oversight. And he was also very open to the non-Western and nonscientific uses of psychedelics, which was unusual among white-lab-coat-wearing 1950s scientists.” Breen observes that the challenge of treating the mental-health effects of World War II on soldiers — what we now call PTSD — absorbed psychiatrists in an age before modern antidepressants. “Psychedelics were the shiny new thing, and LSD was one of the first substances to be seen as a cure for the age of postwar trauma and anxiety that we’re all still kind of living in.”
It was Cohen, Breen surmises, who introduced LSD to the playwright and politician Clare Booth Luce and her husband, Henry Luce, publisher of Time and Life — which led to plenty of psychedelic-positive press, most famously a 1957 first-person essay in Life called “Seeking the Magic Mushroom,” by R. Gordon Wasson 1920JRN. “We chewed and swallowed these acrid mushrooms, saw visions, and emerged from the experience awestruck,” wrote Wasson, a vice president at J. P. Morgan who had traveled to a remote village in southern Mexico with his mushroom-hunter wife and a Life photographer — the original psychedelic tourists. There, a curandera, or healer, introduced them to an ancient religious rite unknown to the West. Nothing had prepared Wasson for what he called the “astonishing effects of the mushrooms,” which provided a “beatific sense of awe and ecstasy.”
But the popularity in the early 1960s of Timothy Leary, the Harvard psychologist who encouraged young people to “turn on, tune in, drop out,” raised alarm among doctors. Cohen, for one, worried that the drug was being mishandled by recreational users who erroneously believed that simply by taking LSD and having “seen the glory,” they had nothing further to do. “LSD isn’t an end, it’s a beginning,” Cohen insisted at a talk at UCLA in 1966. “It’s an opportunity for change. It’s not change itself.”
Then there was Harold Abramson 1920CC, 1923VPS, a prominent New York allergist who wrote about the therapeutic benefits of LSD and who, as reported in Luce’s Time in 1955, hosted dinner parties topped off by a dose of the drug in a liqueur glass: “Instead of upsetting the subjects,” the article read, “it often helps them to recall and relive — in each other’s presence — experiences and emotions of childhood that previously had been too painful to face.”
But Abramson’s activities had another side. Abramson had worked on chemical weapons during the war, and now the CIA, in a Cold War Spy vs. Spy quest for a mind-control advantage against the Soviets, funded Abramson’s research on LSD (it was thought to hold promise as a truth serum). That research, some of which he carried out at Columbia, came to the attention of anthropologist Margaret Mead 1923BC, ’28GSAS, ’64HON, one of America’s best-known public intellectuals. Mead had been acquainted with psychedelics since at least 1930, when she attended a peyote ceremony with the Omaha tribe in Nebraska.
“Mead saw psychedelics as something that could help people to adapt to the rapid pace of modern life and to integrate different aspects of the culture,” says Breen. “She was seeking a conceptual vocabulary for psychedelics that didn’t just see them as traditional practices.”
Mead expressed strong interest to Abramson in trying LSD, but Breen hasn’t found definitive evidence that she went through with it. He speculates that Mead may have feared that secrets about her same-sex relationships might come out while she was drugged. That was apart from the legal risks: by the time Mead died in Manhattan in 1978, New York’s draconian Rockefeller drug laws were in effect, and anyone caught with as little as five milligrams of LSD — about fifty doses — faced a mandatory minimum sentence of one to eight years in prison.
Though psychedelics are still illegal at the federal level, the glowing results of clinical trials across the psychedelic spectrum portend an array of FDA-approved treatments in the future. All of which leads to bigger questions: Who will have access to these treatments and who won’t? Who will benefit and who will be left behind?
For Heidi Allen, an associate professor at the School of Social Work, access and affordability are key. Allen, who studies health care among low-income populations, wants to instill social-work values in the profit-conscious world of prescription-drug coverage and trendy therapies. “When you bring innovations in mental health into the US health-care system,” she says, “it can often widen existing disparities, which are even more pronounced when it comes to specialized mental-health care.”
Allen recently created the School of Social Work’s Psychedelic Therapy Training Program — the first such program in the world to be offered within a graduate professional degree. Social workers play a vital role in mental-health care: they can provide talk therapy and are often on the front lines of mental-health interventions. Allen wants to prepare them for the psychedelic wave, to ensure that the new treatments aren’t confined to boutique medical clinics. “The people who need the treatments the most — even if they are poor or uninsured — should be first to receive them,” Allen says.
This fall, the program’s inaugural cohort of twenty embarked on a novel educational journey. Students take four electives focused on psychedelic-assisted therapy and must also complete a six-hundred-hour practicum in clinics in New York providing ketamine-assisted therapy, including Columbia’s ketamine program, which is led by Jeffrey Zabinski, the assistant director of interventional psychiatry at CUIMC.
Ketamine is not a psychedelic but rather an FDA-approved anesthetic. At smaller doses, it yields certain psychedelic effects and has become a last resort for patients who have fruitlessly tried other treatments for depression. “Usually within the first four to six weeks we see a fairly good response for the majority of patients,” Zabinski says, “and a good number of them go all the way to remission.” Columbia’s clinic administers both a nasal spray (esketamine, a few molecules removed from ketamine) and intravenous ketamine infusions, which will give the social-work students a fair idea of what to expect when full-fledged psychedelic-assisted therapy arrives. Zabinski, who in addition to an MD has a master’s in social work, welcomes the revolution.
“The hope is that patients who are suffering from conditions that previously were extremely difficult to treat will be able to access relief much more quickly,” he says. “The idea of having something you could do in an office-based setting that has a good safety profile and that reaches the level of effectiveness that we’re seeing in these clinical trials — that would be totally transformational.”
Meanwhile, the studies keep coming. At Columbia, chemist David Lankri, a researcher in the lab of chemistry professor Dalibor Sames, has synthesized the psychedelic compound found in the poison of the Sonoran Desert toad, which he believes could someday treat anxiety and depression without activating the brain’s psychedelic receptors (an alternative for those who would rather not visit the unknown interior). And Jae Sevelius, a professor of medical psychology who has studied the effects of psilocybin on long-term AIDS survivors, is conducting two new studies: one on psychedelic drug use among transgender and gender-nonconforming people to explore how these substances affect identity and self-acceptance, and another on ketamine-assisted therapy in a group setting at the Columbia Department of Psychiatry.
As someone who treats vulnerable groups, Sevelius is especially sensitive to the concerns that troubled clinicians sixty years ago: that without regulation, underground demand for the drugs will increase, along with the risks posed by harmful additives, negative interactions with other medications, and difficult psychoactive experiences. “Because there has been so much coverage about the promise of psychedelics to treat these intractable mental-health issues — and because we have such a terrible mental-health-care system where people aren’t getting treatment — I worry that people will take these medicines on their own, or with someone posing as a psychedelic-assisted therapist, and not get the sort of guidance they truly need,” Sevelius says.
That worry is compounded by the likelihood that depression and anxiety rates won’t decline anytime soon. The long march of psychedelics to the verge of FDA approval comes at a time of widespread suffering, and Hellerstein hopes the government will help expedite psychedelic research by funding more robust clinical trials and exploratory studies, as it does for other drugs.
“Are psychedelics really as good as people believe they are?” Hellerstein says. “I would say that the question itself is an argument for government-funded studies, because if the drugs don’t work, or they’re toxic or cause other problems, that would be important to know. But they may also be paradigm-changing in terms of our understanding of effective treatments.
“So the National Institutes of Health should fund more of this research. And if the findings turn out to be less positive than we’d hoped for, that would be interesting too: the point is that you want really good research to find out the actual benefits and risks. You don’t want everything to be done by enthusiasts and proselytizers.”
The Spiritual Roots of Peyote
For thousands of years, Indigenous people in Mexico have been harvesting psychedelic mushrooms and plants and ingesting them in religious ceremonies. One of these plants, peyote, a cactus native to northern Mexico, contains the hallucinogenic compound mescaline, which has long been central to rituals of the Wixárika people, who live in the Sierra Madre Occidental mountains in Jalisco as well as the states of Durango, Zacatecas, and Nayarit. Preserved peyote found in caves in Mexico has been carbon-dated to 4000 BC.
By the late nineteenth century, peyote, largely criminalized in North America (European colonists saw the rites as idolatrous, an attitude that persisted after independence), had spread to tribes in the US. In 1918, Indigenous peyotists in the Oklahoma Territory formed the intertribal Native American Church to give legal protection to their ceremonies.
Meanwhile, Western anthropologists and physicians had discovered the plant’s psychotropic powers. “From the start, the Wixárika have taken in sick Westerners, researchers, and Native Americans, and taught them about peyote,” says anthropologist Estrella Castillo ’19GS, a PhD candidate at Yale who studies the intersections of psychedelics, Indigenous knowledge, religion, and environmental justice. Castillo worries that the current hype around psychedelic-assisted therapy is boosting demand for mescaline — at the expense of the Wixárika.
With Westerners, she says, “there is an extractive relationship, including the borrowing of cultural elements.” She adds that tribal elders are willing to share their knowledge, so long as the substance is “neither vulgarized nor burglarized: the elders ask that their rituals and knowledge not be borrowed without prior consent; that an elder be present to facilitate the healing ceremony, the transmission of prayers, and safeguard from potential harm; and that the medicine be ethically sourced.”
But the most recent big threat to the Wixárika medicinal practices, says Castillo, are the drug cartels that have infiltrated peyote fields in Mexico, speeding up the harvest to feed the black market and exacerbating land-use conflicts and environmental threats from industrial agricultural. Castillo wants to see a more localized psychedelic ecosystem, with more medical research into LSD, which can be made cheaply in a lab. For her, peyote is no mere commodity.
“Peyote is a reinforcer of indigeneity,” she says. “It connects Indigenous diasporic people like myself and gives us a way of remaining connected to the land of our ancestors.”
This article appears in the Fall 2024 print edition of Columbia Magazine with the title "The Psychedelic Prescription."