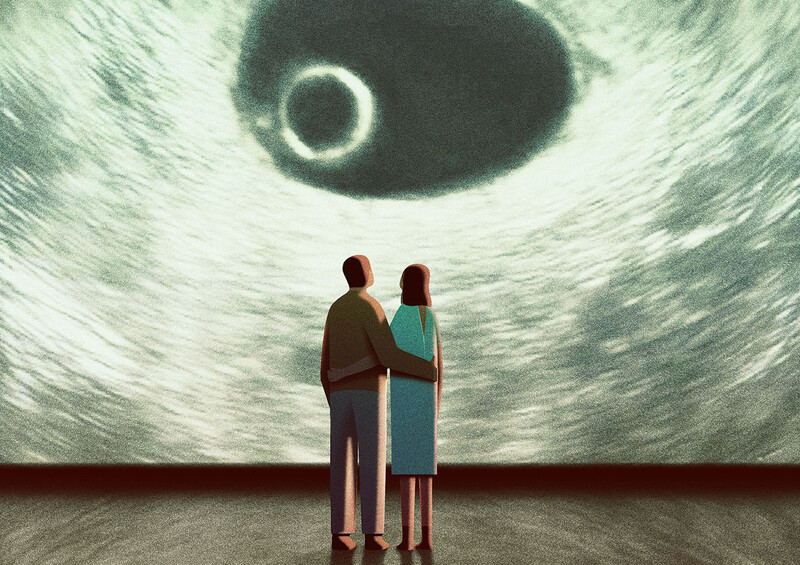
Precision medicine is reshaping the health-care field, as doctors and researchers use patients’ genetic profiles to choose the treatments that are likely to work best for them.
But for all its promise, precision — or personalized — medicine is also poised to create new inequities. That’s because the people who have had their DNA collected as part of medical-research projects are disproportionately white. This means that some conclusions drawn from genetic databases may apply only to white people, since diseases can present differently from one ethnic group to another — progressing at different speeds and responding differently to treatments.
Sandra Soo-Jin Lee, an anthropologist and bioethicist in the recently created Department of Medical Humanities and Ethics at Columbia University Irving Medical Center (CUIMC), is hoping to address the imbalance by leading a four-year, $2.8 million study to identify the most effective ways of increasing minority-group participation in DNA-collection efforts. Funded by the National Human Genome Research Institute, her project will evaluate efforts now being undertaken at academic medical centers across the US, including at CUIMC, to build more diverse genetic databases.
“Without engaging underrepresented communities in genetic studies, efforts to move precision science forward may recapitulate ongoing inequalities in health care and bias the research,” Lee says. “The early stages of precision medicine offer a critical window in which to intervene before research practices and their consequences become locked in.”
She warns that diversifying genetic databases may prove challenging, however. “There is a long history of racial discrimination and exploitation in medical research,” she says. “Questions about trust loom large.”